Scientists have created a detailed cellular and molecular map of the healthy human heart to understand how this vital organ functions and to shed light on what goes awry in cardiovascular disease.
The work, published in Nature Sept. 24 was led by investigators at Harvard Medical School, Brigham and Women’s Hospital, the Wellcome Sanger Institute, Max Delbrück Center for Molecular Medicine (MDC) in Germany, Imperial College London and their global collaborators.
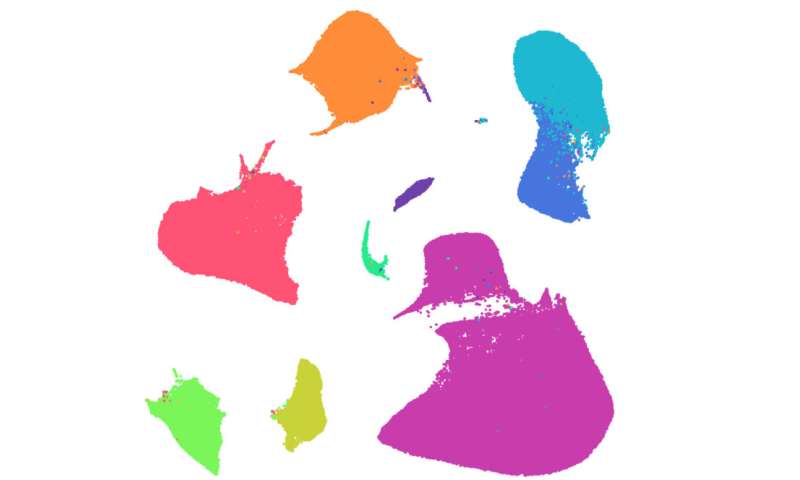
The team analyzed almost a half million individual cells to build the most extensive cell atlas of the human heart to date. The atlas shows the huge diversity of cells and reveals heart muscle cell types, cardiac protective immune cells and an intricate network of blood vessels. It also predicts how the cells communicate to keep the heart working.
The research is part of the Human Cell Atlas initiative to map every cell type in the human body. The new molecular and cellular knowledge of the heart promises to enable better understanding of heart disease and guide the development of highly individualized treatments.
The work also sets the stage for therapies based on regenerative medicine in the future, the researchers said.
Over a lifetime, the average human heart delivers more than 2 billion life-sustaining beats to the body. In doing so, it helps deliver oxygen and nutrients to cells, tissues and organs and enables the removal of carbon dioxide and waste products. Each day, the heart beats around 100,000 times with a one-way flow through four different chambers, varying speed with rest, exercise and stress. Every beat requires an exquisitely complex but perfect synchronization across various cells in different parts of heart. When this complex coordination goes bad, it can result in cardiovascular disease, the leading cause of death worldwide, killing an estimated 17.9 million people each year.
Detailing the molecular processes inside the cells of a healthy heart is critical to understanding how things go awry in heart disease. Such knowledge can lead to more precise, better treatment strategies for various forms of cardiovascular illness.
“Millions of people are undergoing treatments for cardiovascular diseases. Understanding the healthy heart will help us understand interactions between cell types and cell states that can allow lifelong function and how these differ in diseases,” said study co-senior author Christine Seidman, professor of medicine in the Blavatnik Institute at Harvard Medical School and a cardiovascular geneticist at Brigham and Women’s.
“Ultimately, these fundamental insights may suggest specific targets that can lead to individualized therapies in the future, creating personalized medicines for heart disease and improving the effectiveness of treatments for each patient,” Seidman said.
This is what researchers set out to do in the new study.
The team studied nearly 500,000 individual cells and cell nuclei from six different regions of the heart obtained from 14 organ donors whose hearts were healthy but unsuitable for transplantation.
Using a combination of single-cell analysis, machine learning and imaging techniques, the team could see exactly which genes were switched on and off in each cell.
The researchers discovered major differences in the cells in different areas of the heart. They also observed that each area of the heart had specific subsets of cells—a finding that points to different developmental origins and suggests that these cells would respond differently to treatments.
“This project marks the beginning of new understandings into how the heart is built from single cells, many with different cell states,” said study co-first author Daniel Reichart, research fellow in genetics at Harvard Medical School. “With knowledge of the regional differences throughout the heart, we can begin to consider the effects of age, exercise and disease and help push the field of cardiology toward the era of precision medicine.”
“This is the first time anyone has looked at the single cells of the human heart at this scale, which has only become possible with large-scale single-cell sequencing,” said Norbert Hübner, co-senior author and professor at Max Delbrück Center for Molecular Medicine. “This study shows the power of single-cell genomics and international collaboration,” he added. “Knowledge of the full range of cardiac cells and their gene activity is a fundamental necessity to understand how the heart functions and to start to unravel how it responds to stress and disease.”
As part of this study, the researchers also looked at blood vessels running through the heart in unprecedented detail. The atlas showed how the cells in these veins and arteries are adapted to the different pressures and locations and how this could help researchers understand what goes wrong in blood vessels during coronary heart disease.
“Our international effort provides an invaluable set of information to the scientific community by illuminating the cellular and molecular details of cardiac cells that work together to pump blood around the body,” said co-senior author Michela Noseda of Imperial College, London. “We mapped the cardiac cells that can be potentially infected by SARS-CoV-2 and found that specialized cells of the small blood vessels are also virus targets,” she said. “Our datasets are a goldmine of information to understand subtleties of heart disease.”
The researchers also focused on understanding cardiac repair, looking at how the immune cells interact and communicate with other cells in the healthy heart and how this differs from skeletal muscle.
Further research will include investigating whether any heart cells could be induced to repair themselves.
“This great collaborative effort is part of the global Human Cell Atlas initiative to create a ‘Google map’ of the human body,” said Sarah Teichmann of the Wellcome Sanger Institute, co-senior author of the study and co-chair of the Human Cell Atlas Organising Committee.
Source: Read Full Article


