Peripheral artery disease affects 8–10 million people in the U.S., most over age 65. But it also affects younger people who have additional risk factors, such as diabetes, smoking, obesity and high blood pressure. Also, 30% of Black Americans will develop peripheral artery disease, compared to 20% each from non-Hispanic white, Hispanic or Native American backgrounds.
Dr. Amy Pollak, a Mayo Clinic cardiologist, explains how physicians identify peripheral artery disease and why an early diagnosis can reduce the risk of amputation, heart attack and stroke.
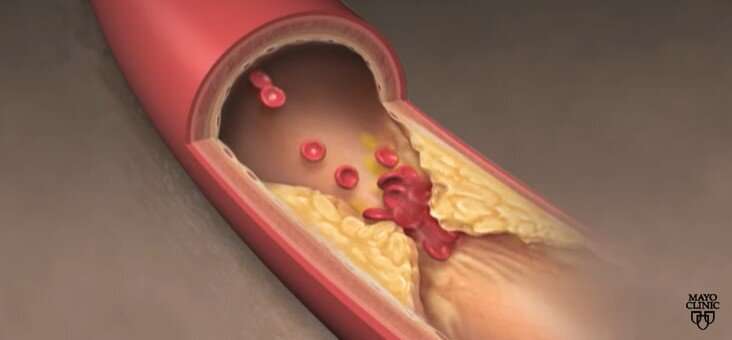
Peripheral artery disease involves cholesterol buildup in arteries or blood vessels of the legs. The condition can restrict blood flow and lead to complications.
“Peripheral artery disease not only influences our ability to walk, but it puts us at a risk for amputation,” says Dr. Pollak. “And that also ties in with heart attack and stroke because of systemic cholesterol buildup.”
Diagnosing peripheral artery disease starts by checking circulation to the feet.
“Taking off the shoes and socks, doing a foot exam, feeling the pulses, and then, if you have somebody who either has symptoms that are concerning or an abnormal pulse exam, the next diagnostic test is something that’s straightforward to do,” says Dr. Pollak.
An ankle-brachial index test can identify circulation issues by comparing blood pressure in a person’s ankle to that in their arm before and after exercise. Tests and time with a health care team can promote conversations about the most appropriate medical treatment.
“Not only do we typically think of cholesterol medications, such as statins or the role of aspirin, but some of the other medications to help reduce that future risk,” says Dr. Pollak.
https://youtube.com/watch?v=ugeQAhDWU4M%3Fcolor%3Dwhite
Source: Read Full Article