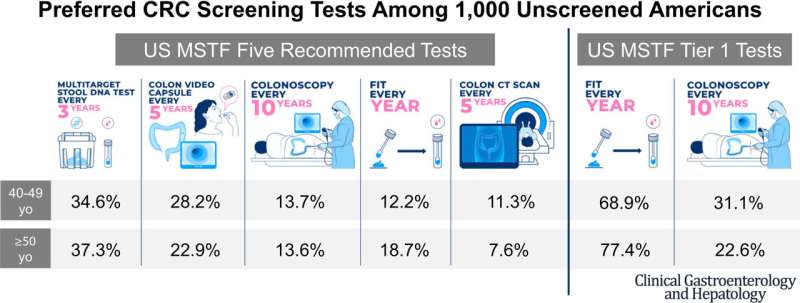
Three-quarters of people prefer to do a fecal immunochemical test (FIT) rather than a colonoscopy for their regular colorectal cancer screening, according to a new Cedars-Sinai study.
Unlike colonoscopies, FIT doesn’t require lengthy preparation, diet changes or sedation. Patients are asked to simply provide a stool sample using a test kit, which can be mailed to their home or picked up at the lab.
“One of the big issues is that many people think colorectal cancer screening and colonoscopy are synonymous, and that the only way to get screened for colorectal cancer is through a colonoscopy,” said Christopher V. Almario, MD, MSHPM, assistant professor of Medicine and corresponding author on the study. “In fact, there are many different ways to get tested.”
Understanding that there are more options like the less-time-consuming and less-invasive FIT could persuade more people to get lifesaving screenings. This is especially important since one-third of Americans are not up to date on their colorectal cancer screenings, noted Almario. And in 2021, the U.S. Preventive Services Task Force lowered the recommended age for colorectal cancer screening to 45.
For the study, published this month in the peer-reviewed journal Clinical Gastroenterology and Hepatology, Almario’s team surveyed 1,000 people ages 40 years or older who had not already been screened for colorectal cancer. Participants considered the top two tests recommended by a multi-society task force made up of representatives from the nation’s leading gastroenterology medical societies:
- Yearly FITs
- Colonoscopies every 10 years
When choosing between the two tests, about three-quarters of people preferred the yearly FIT over a colonoscopy every 10 years for their colorectal cancer screening.
“With the FIT test, there’s no change of diet, no anesthesia, and you can do it at home,” Almario said. “If it’s negative, then you repeat it a year later. If it’s positive, you do need to come in and get a colonoscopy so we can find the cancer if it’s there as well as remove any pre-cancerous polyps.”
Interestingly, Almario notes that investigators were unable to predict which screening method participants preferred based on their demographics and clinical characteristics.
“I think this just shows that everyone is different,” Almario said. “As clinicians, we simply need to ask patients which test they want to do, because the best test is the test that actually gets done.”
Almario’s team is now testing education and decision-aid materials that may guide patients’ decision making when choosing which screening method is right for them.
Source: Read Full Article