A new study conducted by researchers at the University of Eastern Finland discovered that the APP A673T genetic variant, which protects against Alzheimer’s disease, alters levels of several proteins and peptides linked to amyloid-beta metabolism in human biofluids and cell culture models, including amyloid beta itself. These new data support the idea that even a modest reduction in the beta-amyloidogenic processing of APP may be a feasible strategy for the prevention of Alzheimer’s disease.
Alzheimer’s disease (AD) is the most common form of dementia with more than 40 million affected people worldwide. Two of the key pathological features of AD are amyloid plaques, composed of toxic amyloid-beta (Aβ) peptides, and neurofibrillary tangles, consisting of hyperphosphorylated tau protein. Although these molecular characteristics have been known for decades, there have been many setbacks in the development of therapies for an effective prevention or treatment of AD.
However, recent clinical trials targeting different steps of Aβ aggregation have shown promise in slowing down the disease progression. Aβ is part of the amyloid precursor protein (APP) and it is generated upon the sequential proteolytic cleavage of APP. In 2012, researchers from Iceland discovered a genetic variant within the APP gene that protects its carriers from AD. Consequently, a previous study conducted at the University of Eastern Finland found that carriers of the APP A673T variant show lower levels of Aβ in the plasma as compared to control individuals. As the discovered APP A673T variant is very rare and almost exclusively found in Nordic populations, there are only a few studies on its effects and mechanisms.
In the present study, published in Neurobiology of Disease, the researchers analyzed cerebrospinal fluid (CSF) and plasma of APP A673T carriers and control individuals using mass spectrometry-based proteomics, which allows the identification of changes in protein levels between the study groups in an unbiased manner. Furthermore, the APP A673T variant was introduced into 2D and 3D neuronal cell culture models together with pathogenic APP mutations.
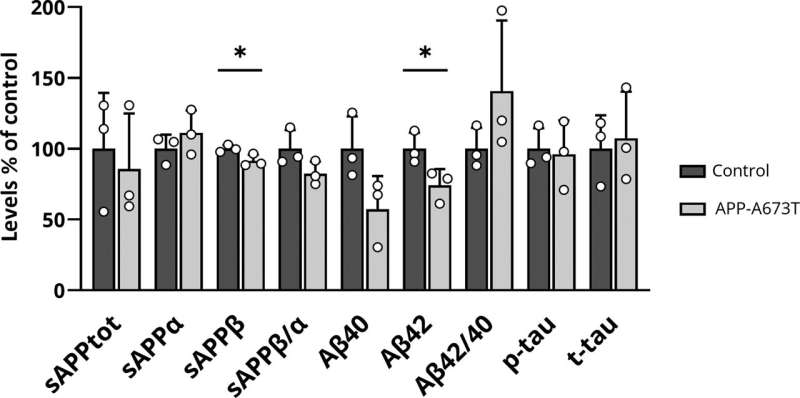
The study reports for the first time the protective effects of the APP A673T variant against AD-related alterations in the CSF, plasma, and brain biopsy samples from carriers of the genetic variant. The CSF levels of Aβ42 and soluble APP-beta (sAPPβ), which is another metabolite of beta-amyloidogenic processing of APP, were significantly decreased in APP A673T carriers as compared to well-matched controls not carrying the protective variant.
The unbiased proteomics approach from CSF and plasma samples of APP A673T carriers identified differences in the levels of several proteins and peptides that are intimately involved in protein phosphorylation, inflammation, and mitochondrial function. Importantly, some of the identified key targets showed inverse correlation in the postmortem brain tissue from AD patients in relation to the severity of the disease.
In 2D and 3D neuronal cell culture models expressing two strong AD-causing APP mutations, the introduction of the APP A673T variant resulted in robust changes in APP processing products. In line with the results from CSF, particularly the levels of sAPPβ were lower in all the models expressing APP A673T, often accompanied by decreased levels of Aβ42. These results demonstrate the effectiveness of the protective APP A673T variant to shift APP processing from beta-amyloidogenic toward the non-amyloidogenic pathway even in the presence of two pathogenic APP mutations.
In summary, these findings emphasize that even a modest reduction in the beta-amyloidogenic processing of APP could be a feasible strategy for the prevention of AD. Furthermore, unbiased proteomics analyses highlighted specific targets and pathways, which may play a key role in AD progression.
More information:
Rebekka Wittrahm et al, Protective Alzheimer’s disease-associated APP A673T variant predominantly decreases sAPPβ levels in cerebrospinal fluid and 2D/3D cell culture models, Neurobiology of Disease (2023). DOI: 10.1016/j.nbd.2023.106140
Journal information:
Neurobiology of Disease
Source: Read Full Article


