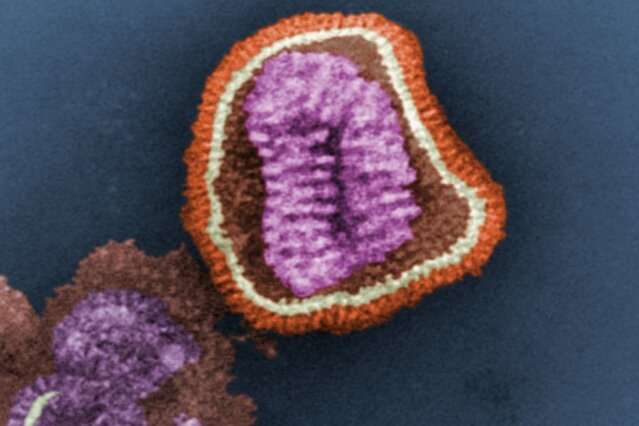
While the incidence of influenza-associated neuropsychiatric events in children in the United States is unknown, the controversy over the use of a common antiviral medication typically administered to treat flu in children has sparked concern among parents and medical professionals alike.
The dilemma about whether the treatment causes neuropsychiatric events or if the infection itself is the culprit, led a group of pediatric researchers at Monroe Carell Jr. Children’s Hospital at Vanderbilt to study the question.
“Population-Based Incidence of Influenza-Associated Serious Neuropsychiatric Events in Children” published in JAMA Pediatrics examines how often children diagnosed with flu experience serious neuropsychiatric side effects.
“We are among the first to quantify these serious events in the pediatric population in the United States,” said principal investigator James Antoon, MD, Ph.D., MPH, assistant professor of Pediatrics and Hospital Medicine at Monroe Carell. “We knew some of the neurological events occurred, but we did not know how often and in whom.”
“Our study quantified the number of pediatric neuropsychiatric events, described which children are more likely to experience the events and showed that these events occur in both those children treated and not treated with an antiviral. Ongoing studies will help us assess if use of influenza antivirals is associated with the risk of neuropsychiatric events in children,” Antoon said.
“This study highlights the importance of understanding the frequency and context in which neuropsychiatric events occur … especially among young children and children with underlying conditions who are also at high risk for influenza complications,” said senior author Carlos Grijalva, MD, MPH, professor of Health Policy and Biomedical Informatics at Vanderbilt University Medical Center.
According to the study, Oseltamivir, known as Tamiflu, has a black box warning about neuropsychiatric side effects. Previous studies have been mixed on whether using Tamiflu causes these events.
“This potential side effect makes headlines every influenza season and is often a concern for parents and providers, who weigh the risk of these events when making the decision to treat with antivirals,” said Antoon. “Our findings show that influenza infection itself can be associated with neuropsychiatric events, and that should be part of the conversation when counseling families.”
In a retrospective cohort study, researchers used the Tennessee Medicaid database to identify children ages 5-17 years with an outpatient diagnosis of flu during 2016-2020.
A total of 156,661 flu diagnoses were included. Findings showed that rates were higher among adolescents, in those with risk factors for flu complications and were 10- and 100-times higher in children with neurologic and psychiatric disorders.
Neurologic events include seizures, encephalitis, altered mental status, ataxia/movement disorders, vision changes, dizziness and headache. Psychiatric events consist of homicidal, suicidal, self-harm behaviors, mood disorders and psychosis/hallucination).
“Fortunately, the most serious events, such as suicidal and self-harm behaviors, as well as encephalitis, were rare,” said fellow researcher Derek Williams, MD, MPH, chief of the Division of Hospital Medicine at Monroe Carell. “Nonetheless, each of these events is of concern, regardless of severity. It’s also likely that many of these complications could be avoided with influenza vaccination.”
More information:
James Antoon et al, Population-Based Incidence of Influenza-Associated Serious Neuropsychiatric Events in Children, JAMA Pediatrics (2023). DOI: 10.1001/jamapediatrics.2023.2304. jamanetwork.com/journals/jamap … cle-abstract/2807627
Journal information:
JAMA Pediatrics
Source: Read Full Article