A novel therapeutic approach that combines human epidermal growth receptor factor 2 (HER2)-targeted therapies with the cholesterol-lowering drug lovastatin can reduce the number of cancer treatments required to prevent tumor growth. Monitored by immuno-PET scans, this combination therapy has the potential to personalize treatment for cancer patients and spare them from harmful side effects.
This research was published in the October issue of The Journal of Nuclear Medicine.
Antibody-drug conjugates (ADCs) have become an eminent cancer treatment because of their ability to precisely target tumors with potent efficacy. HER2-ADC therapies have been effective in treating breast, lung, bladder, and stomach cancers. Although they are usually well-tolerated, multiple doses of the drugs can result in severe side effects, including low blood counts, liver damage, and lung damage. Strategies that reduce toxic side effects caused by ADCs and predictive biomarkers of ADC toxicity are currently an unmet clinical need.
“In this study, we sought to determine whether a single dose of HER2-ADCs could be administered in combination with lovastatin (which temporarily elevates cell-surface HER2) to achieve therapeutic efficacy similar to that of a multiple dose regime,” said Patricia Pereira, Ph.D., assistant professor at the Mallinckrodt Institute of Radiology at the Washington University School of Medicine in St. Louis, Missouri. “We also used HER2-targeted immuno-PET to monitor changes in HER2 expression after ADC therapy.”
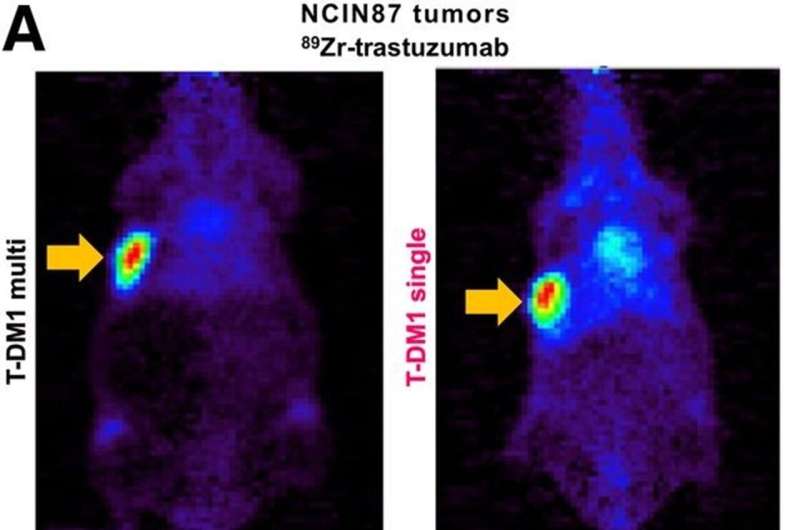
Researchers injected mice with cultured gastric cancer cells and patient-derived gastric cancer cells. When tumors grew sufficiently, the mice were divided into groups and received various treatment schedules (no treatment, multiple doses of ADC, multiple doses of ADC with lovastatin, single dose of ADC, or single dose of ADC with lovastatin). Immuno-PET was used to investigate the dosing regimen and the efficacy of the treatment schedules.
A single dose of ADC therapy combined with lovastatin was found to reduce tumor volume at rates similar to those resulting from multiple doses of ADC in a preclinical setting. The study results showed that immuno-PET can noninvasively monitor HER2 tumor levels after treatment with HER2-targeted ADC therapies.
“This preclinical work is significant because it has the potential to improve therapy for patients with HER2-positive cancers,” noted Pereira. “It not only simplifies treatment by exploring single-dose schedules of antibody-drug conjugates but can also reduce side effects by minimizing the number of doses required. Additionally, it personalizes therapy using molecular imaging, enhancing treatment efficacy.”
She continued, “The findings suggest a future where molecular imaging techniques play a critical role in guiding drug development and cancer treatment decisions, particularly as various ADCs are being tested and approved for cancer treatment. Currently, there is no perfect way to select tumors or monitor their response to ADCs. This research indicates that molecular imaging can bridge this gap by providing real-time insights into therapy response.”
More information:
Emma L. Brown et al, Immuno-PET Detects Antibody–Drug Potency on Coadministration with Statins, Journal of Nuclear Medicine (2023). DOI: 10.2967/jnumed.122.265172
Journal information:
Journal of Nuclear Medicine
Source: Read Full Article


