Diabetic patients whose natural wound-healing capabilities are compromised often develop chronic wounds that are slow to heal. Such non-healing wounds could cause serious infections resulting in painful outcomes, such as limb amputation. To address this global health care challenge, a team of researchers from the National University of Singapore (NUS) engineered an innovative magnetic gel that promises to accelerate the healing of diabetic wounds, reduce the rates of recurrence, and in turn, lower the incidents of limb amputations.
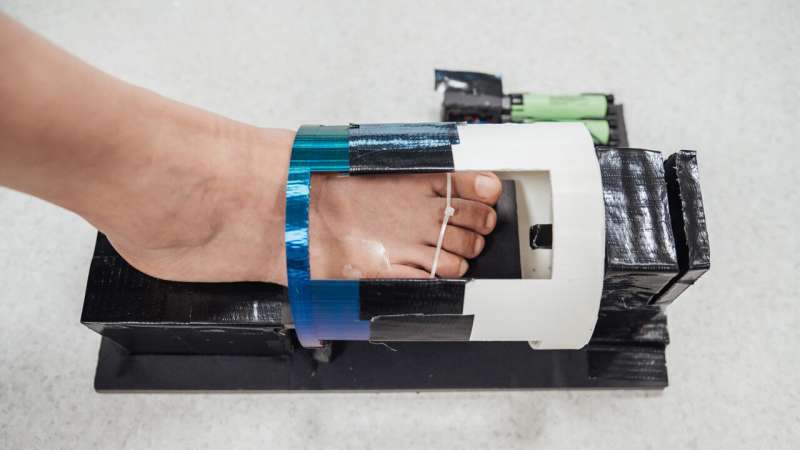
Each treatment involves the application of a bandage pre-loaded with a hydrogel containing skin cells for healing and magnetic particles. To maximize therapeutic results, a wireless external magnetic device is used to activate skin cells and accelerate the wound healing process. The ideal duration of magnetic stimulation is about one to two hours.
Lab tests showed the treatment coupled with magnetic stimulation healed diabetic wounds about three times faster than current conventional approaches. Furthermore, while the research has focused on healing diabetic foot ulcers, the technology has potential for treating a wide range of complex wounds such as burns.
“Conventional dressings do not play an active role in healing wounds,” said Assistant Professor Andy Tay, who leads the team comprising researchers from the Department of Biomedical Engineering at NUS College of Design and Engineering as well as the NUS Institute for Health Innovation & Technology. “They merely prevent the wound from worsening, and patients need to be scheduled for dressing change every two or three days. It is a huge cost to our health care system and an inconvenience to patients.”
In contrast, the unique NUS invention takes a comprehensive “all-in-one” approach to wound healing, accelerating the process on several fronts.
“Our technology addresses multiple critical factors associated with diabetic wounds, simultaneously managing elevated glucose levels in the wound area, activating dormant skin cells near the wound, restoring damaged blood vessels, and repairing the disrupted vascular network within the wound,” explained Tay.
The NUS team described their innovation in a paper published in the scientific journal Advanced Materials, on 8 September 2023.
Chronic diabetic wounds: A major health care challenge
Currently, more than half a billion people globally are living with diabetes and this number is expected to rise significantly. Chronic diabetic wounds such as foot ulcers (one of the most common and hardest to treat wounds) have therefore become a major global health care challenge.
Traditional treatments for these wounds are often unsatisfactory, leading to recurring and persistent health issues and—in a high number of cases—limb amputation.
Every year, there are around 9.1 to 26.1 million cases of diabetic foot ulcer worldwide, and around 15% to 25% of patients with diabetes will develop a diabetic foot ulcer during their lifetime. Singapore has one of the highest rates of lower limb amputation due to diabetes globally, averaging around four per day.
Gentle ‘work-out’ for skin cells
Skin cells experience mechanical forces continuously from normal daily activities. However, patients with wounds are usually advised not to carry out rigorous activities, such as walking, as this could kill the remaining cells essential for healing.
“What our team has achieved is to identify a sweet spot by applying gentle mechanical stimulation,” said Tay. “The result is that the remaining skin cells get to ‘work-out’ to heal wounds, but not to the extent that it kills them.”
The specially designed wound-healing gel is loaded with two types of FDA-approved skin cells—keratinocytes (essential for skin repair) and fibroblast (for formation of connective tissue)—and tiny magnetic particles. When combined with a dynamic magnetic field generated by an external device, the mechanical stimulation of the gel encourages dermal fibroblasts to become more active.
Lab tests showed that the increased fibroblast activity generated by the magnetic wound-healing gel increases the cells’ growth rate by approximately 240% and more than doubles their production of collagen—a crucial protein for wound healing. It also improves communication with keratinocytes to promote the formation of new blood vessels.
“The approach we are taking not only accelerates wound healing but also promotes overall wound health and reduces the chances of recurrence,” added Tay.
The NUS team work on the project from 2021 to 2023 to demonstrate the viability of this new approach. A patent has been filed for this innovation.
Potential game-changer in wound management
While the magnetic wound-healing gel has shown great promise in improving diabetic wound healing, it could also revolutionize the treatment of other complex wound types.
“The magneto-responsive hydrogel, combined with wireless magneto-induced dynamic mechanical stimulation, addresses fundamental challenges in wound healing, such as creating a conducive microenvironment and promoting tissue regeneration,” said co-first author of the research paper Dr. Shou Yufeng, Research Fellow from the Department of Biomedical Engineering at NUS College of Design and Engineering.
“These principles and our technology’s adaptability, as well as its general ease of use for patients, means that it can be applied to improve wound healing in various situations beyond diabetes, including burns and chronic non-diabetic ulcers.”
The researchers are conducting more tests to further refine the magnetic wound-healing gel to improve its effectiveness. They are also collaborating with a clinical partner to test the effectiveness of the gel using diabetic human tissues.
“This is major step forward in active wound care,” said Tay. “Our goal is to provide an effective and convenient wound-healing solution that improves outcomes for millions around the world.”
“Wound healing, especially in the field of diabetic foot ulcers, has always been a challenging arena. Diabetic foot patients do not heal as well as normal patients and their healing journey is often prolonged,” said Assistant Professor Francis Wong Keng Lin, Consultant, Department of Orthopaedic Surgery, Sengkang General Hospital.
Wong, who is not involved in the study, added, “Advancements in wound healing technologies will reduce the duration of the patient journey and would allow them to return to their lives as quickly as possible, hence improving productivity and quality of life.”
More information:
Yufeng Shou et al, Mechano‐activated Cell Therapy for Accelerated Diabetic Wound Healing, Advanced Materials (2023). DOI: 10.1002/adma.202304638
Journal information:
Advanced Materials
Source: Read Full Article


