Combining a pair of experimental drugs may help treat malignant peripheral nerve sheath tumors with fewer harmful side effects, according to preliminary animal studies led by investigators at the Johns Hopkins Kimmel Cancer Center and Johns Hopkins Drug Discovery.
The study, published in the journal Molecular Cancer Therapeutics, shows that combining an experimental drug that blocks the metabolism of the amino acid glutamine with a second experimental drug that blocks recycling of purines (building blocks of the genetic material DNA and RNA that tumors need to proliferate) reduced the size of peripheral nerve sheath tumors in mice and increased their rates of survival. The combination was less toxic than previously tested drug combinations.
“Using these broadly active metabolic inhibitors can help us better understand how these tumors are using nutrients to build what they need to make more tumor cells,” says lead study author Kathryn Lemberg, M.D., Ph.D., an assistant professor of oncology at Johns Hopkins.
Malignant peripheral nerve sheath tumors (MPNST) are rare cancers that originate in the lining of the nerves. Individuals with the cancer predisposition syndrome neurofibromatosis type 1 (NF1) have an elevated risk of these cancers. MPNST are the leading cause of death in people with NF1 under the age of 40, Lemberg explains.
“When patients with NF1 develop these tumors, there is, unfortunately, a risk of poor outcome based on whether the tumor can be completely surgically removed, whether it responds to conventional chemotherapy, and how widespread the cancer is,” Lemberg says. “We need better treatments for these tumors.”
Barbara Slusher, Ph.D., M.A.S., director of Johns Hopkins Drug Discovery and senior author on the study, and colleagues developed the glutamine antagonist JHU395 that blocks the utilization of glutamine. JHU395 is particularly well-suited for blocking glutamine metabolism in nerve-associated tissues.
“Glutamine is a building block for proteins and many other large molecules that cancer cells need to grow, proliferate, survive and potentially spread,” Lemberg says.
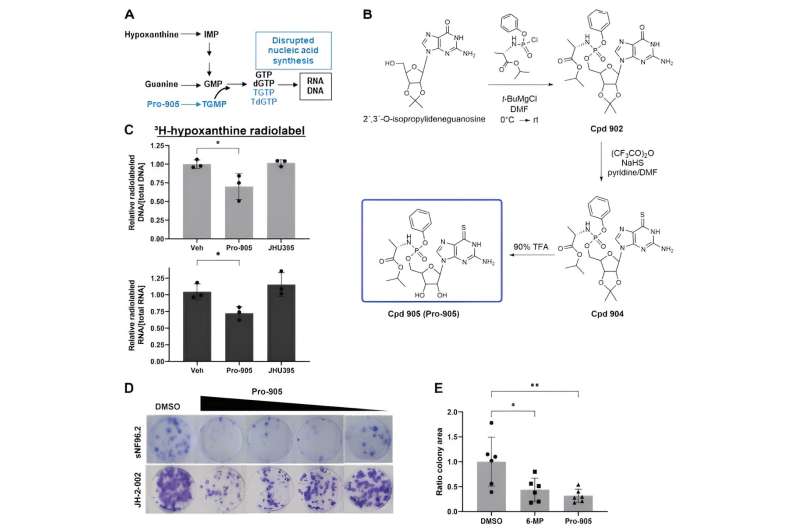
Previous studies by Lemberg, Slusher and colleagues showed that treatent of mouse MPNST with JHU395 yields a partial tumor reduction. The drug works by impairing one arm of purine production, the “de novo” pathway. However, with JHU395 treatment, the tumors can still access purine by a recycling or salvage pathway. Combining JHU395 with the classical purine antimetabolite 6-mercaptopurine (6-MP) produces a better anti-tumor response because 6-MP itself can cause liver and gastrointestinal toxicity based on the way the body metabolizes it to the active form.
Lemberg, Slusher and colleagues from the Institute of Organic Chemistry and Biochemistry (IOCB) of the Czech Academy of Sciences in Prague developed an alternate purine salvage-blocking prodrug called Pro-905. In experiments conducted in collaboration with scientists at Northwestern University, they showed that JHU395 and Pro-905 inhibit purine synthesis in human MPNST cells by distinct mechanisms, leading to decreased synthesis of new DNA and RNA. In mouse models of the condition, they found that Pro-905 in combination with JHU395 reduced tumor growth more effectively than 6-MP and with less toxicity.
“Collaboration is key to moving science forward, particularly for studies of rare tumor types that require the expertise of multiple researchers,” Lemberg says.
Now, Lemberg and colleagues want to see if this experimental drug combination is also effective in other types of tumors that use similar pathways to grow. They also want to test whether this combination might be effective in patients with malignant peripheral nerve sheath tumors or if Pro-905 might be used as maintenance therapy to prevent tumor regrowth, as 6-MP is. Lemberg also plans to collaborate with other Johns Hopkins researchers to determine if starving the tumors of glutamine and purines might also enable the immune system to kick in and fight the tumor.
Earlier research of JHU395 showed that cancer cells steal nutrients, including glutamine, to maintain their survival, starving surrounding cells such as immune cells. Using JHU395 to cut cancer cells off from their supply of glutamine strengthens immune cells, invigorating their response to cancer, Slusher says.
“Building on observations from one study and keeping the science moving forward can open up a lot of potential routes for future therapies for diseases that need better treatment options,” Lemberg says.
More information:
Kathryn M. Lemberg et al, Pro-905, a Novel Purine Antimetabolite, Combines with Glutamine Amidotransferase Inhibition to Suppress Growth of Malignant Peripheral Nerve Sheath Tumor, Molecular Cancer Therapeutics (2023). DOI: 10.1158/1535-7163.MCT-23-0258
Journal information:
Molecular Cancer Therapeutics
Source: Read Full Article