Researchers who have studied malaria for decades, hoping to find a cure, long thought they’d identified a type of blood that seemed to defend against the disease.
But a new study published in Cell Host & Microbe concludes that even some people with the protective blood type became infected. The question now is, how?
“This might mean that the specific gene mutation related to this blood type doesn’t completely stop malaria, or the malaria bug might have found another way to get into the blood cells,” said Peter Zimmerman, a pathology professor at Case Western Reserve University School of Medicine and the study’s senior author. “It’s a big deal because it might change how we try to get rid of this type of malaria parasite.”
“This malaria parasite, called Plasmodium vivax—or P. vivax—used to be common in Northeast Ohio,” said Christopher King, a study co-investigator and pathology professor. “And it was transmitted within the United States—Florida and Texas—this summer for the first time in 20 years.
“We have known,” King said, “that the United States is at risk of re-introduction of malaria with climate changes and increasing immigration and traveling from malaria-endemic areas.”
Study collaborators include researchers from France (Célia Dechavanne and Benoit Gamain, from the National Institute of Blood Transfusion, INSERM/Paris Diderot University); and Madagascar (Arsène Ratsimbasoa, from the University of Fianarantsoa).
The study
“Malaria researchers have been trying to chip away at understanding resistance and susceptibility of P. vivax infection of African people for more than 100 years,” Zimmerman said. “More than 2.5 billion people may live in Africa and Southeast Asia where the parasite is found. Hundreds of thousands of people a year die from malaria. In general, malaria is one of the big three global-health infectious diseases—malaria, tuberculous and HIV/AIDS.”
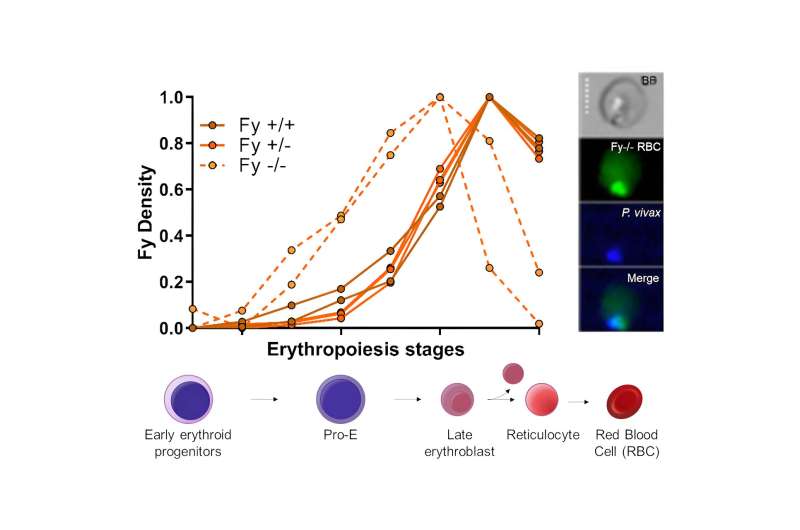
The team is studying a specific blood type (Fy-negative) in the blood of most people in Africa and of African origin, called “the silent Duffy blood group.” Duffy-negative people have a mutation in the DNA code (GATA-1) that results in the protein not being expressed on the surface of red blood cells.
The researchers did experiments using blood cells grown in the lab and cells taken from bone marrow to study the Duffy-silent blood type.
“Surprisingly, we found that even when people are missing the GATA-1 DNA code, the Duffy protein sometimes shows up on their red blood cells,” Zimmerman said. “Our findings suggest that the bone marrow and other places where blood cells are first made are important for the malaria parasite to find the red cells with the Duffy protein, to grow and cause sickness.”
In other experiments in the lab, they examined the blood of people with Duffy silent blood type. They noticed the P. vivax malaria infection was often detected using a special test rather than the usual microscope test.
This means that people with Duffy-silent blood type can still have the infection, but it’s not always easy to see in regular blood tests. In other words, they found that P. vivax can invade the red blood cells of people with the Duffy-silent trait. Also, if they have the infection in the bone marrow, they produce the transmissible form of the parasite. Mosquitoes can acquire it and cause infections in other people.
“This discovery raises questions about how malaria parasites cause infection and sickness, especially because some people with the infection don’t show many signs in their blood,” Zimmerman said. “We need to look at the blood more closely to understand better how widespread and serious this type of malaria is in people with the Duffy-silent trait.”
More information:
Celia Dechavanne et al, Duffy antigen is expressed during erythropoiesis in Duffy-negative individuals, Cell Host & Microbe (2023). DOI: 10.1016/j.chom.2023.10.019
Journal information:
Cell Host & Microbe
Source: Read Full Article


