A study led by Menzies School of Health Research (Menzies) has found a large gap in ear health services provided in remote Northern Territory communities in Australia.
Otitis media (OM) is a bacterial infection and fluid accumulation in the middle ear is linked to ear drum swelling, damage and hearing loss, which can impact a child’s early development. Australian First Nations children have the highest reported rates of OM in the world. In some surveys conducted in remote communities, up to 90% of young Aboriginal children have OM and could have hearing loss.
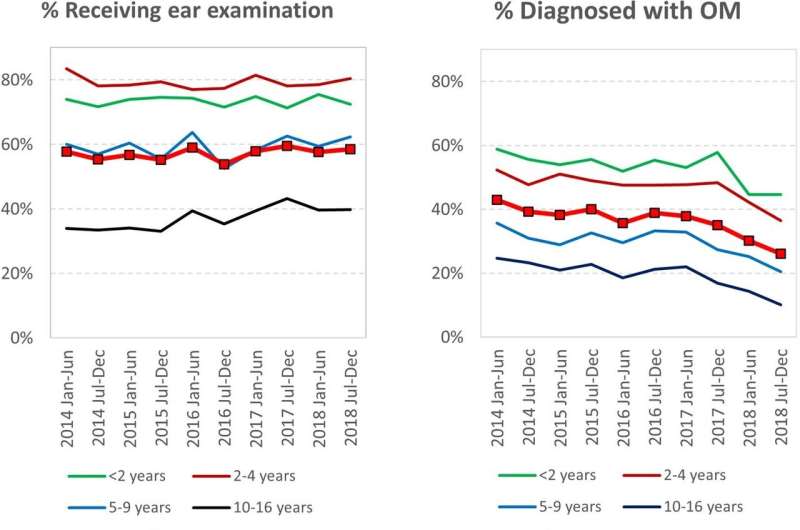
The study found that on average, less than 60% of children aged under 16 years had received an ear check in a 6-month period.
Of those children whose ears were checked, 36% were diagnosed with some type of OM. Out of those children, 90% needed either immediate treatment or a scheduled follow-up. Despite this, just under 25% of that group of children had outcomes of treatment and follow-up recorded.
The study showed that ear health surveillance and compliance in line with OM guidelines (which are endorsed by the Royal Australian College of General Practitioners) were alarmingly low.
Led by Menzies’ researcher Dr. Jiunn-Yih Su, the study findings were recently published in BMC Health Services Research, titled “An evaluation of the quality of ear health services for Aboriginal children living in remote Australia: a cascade of care analysis.”
The research team examined five-year trends in OM prevalence and the quality of ear health services across 50 remote health clinics. They analyzed clinical data from more than 6,000 children between 2014 and 2018.
In a bid to help tackle this issue, Menzies is leading a project which aims to assist in improving ear health of remote children while also up-skilling and creating jobs for a local workforce that fills these identified gaps in the continuity of ear and hearing services.
The Hearing for Learning Initiative (HfLI) is trialing a community-based service enhancement program. Since early 2019, the program has worked for months in each of the 18 communities involved to deliver accredited training and fund employment of Ear Health Facilitators who will work with primary health care and specialists.
The goal is to establish reliable, sustainable and culturally appropriate services that ensure every ear of every child is healthy and hearing every day.
Menzies School of Health Research Data Analyst and lead author, Dr. Jiunn-Yih Su says, “In remote Aboriginal communities in the NT, many children suffer early and persisting otitis media from just a few weeks of age.
“As young children need to hear to learn to speak and communicate, the hearing impairment caused by otitis media has been shown to negatively impact Aboriginal children’s early childhood development, school participation and academic performance.
“These findings reveal many missed opportunities to control high rates of otitis media and to reduce Aboriginal children’s risk of hearing impairment and the associated negative outcomes later in life mentioned above. The Hearing for Learning Initiative is working to close ear and hearing service gaps, to increase ear examinations, improve the effectiveness in diagnosing otitis media, and enhance compliance with otitis media management guidelines which have been designed for First Nations children.”
Source: Read Full Article