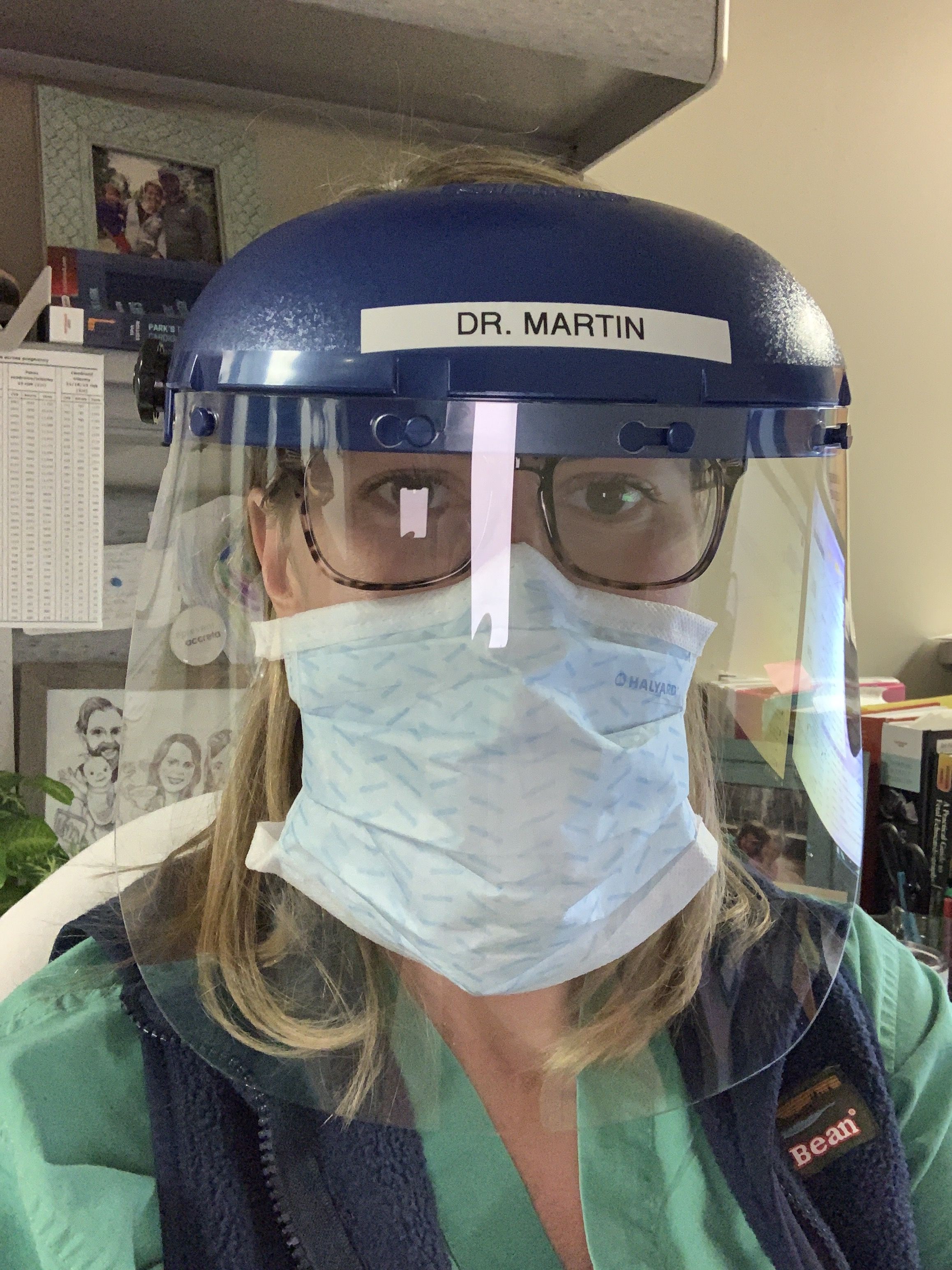
Dr. Jane Martin, MD, is a 34-year-old ob-gyn in New Orleans who delivered her third child January 14. She received her second dose of the Pfizer vaccine on January 6th.
I got the first dose of the Pfizer vaccine when I was 34 weeks and the second at 37 weeks pregnant. After my second dose, Ochsner Health shared a picture of me (visibly pregnant!) getting vaccinated on social, and it went viral. I never expected so much backlash.
All of a sudden, self-proclaimed vaccine experts came out of the woodwork. People from all over the world, who I obviously didn’t know, were commenting with assumptions and judgments about my decision. They had no scientific training or medical background, but all sorts of opinions.
It was disheartening. I was worried that other pregnant women would see the post and all of the backlash that it caused, and it would scare them away from having a conversation with their healthcare providers about potentially receiving the vaccine themselves.
I’m an ob-gyn and specialize in high-risk pregnancies at Ochsner Health.
When the pandemic started last March, we treated some pretty critically ill pregnant patients right away. Our normally sleepy ICU was packed with extremely sick people. Every patient had COVID and was on a ventilator and dialysis. I saw patients around my age, in their thirties and forties, dying of COVID.
Being pregnant during a pandemic was very bittersweet. It made every part of the pregnancy feel a little bit scarier, but it also brought happiness and hope. I have a 5-year-old and a 3-year-old, but emotionally, this pregnancy felt a lot more taxing. Seeing the worst-case scenario, day in and day out didn’t make things easy.

I didn’t expect the COVID-19 vaccine to be available before I delivered.
I was 32 or 33 weeks along when we started hearing about vaccine distribution at work.
I gave myself a crash course on the vaccine to help make a decision for myself and to guide my patients. I knew that the vaccine was expedited in a safe way. And that researchers have been working their entire careers to develop this type of vaccine just for this moment—when a pandemic like the novel coronavirus would emerge.
At first, I was hesitant, just like most pregnant women. I didn’t want to feel like a guinea pig. I wasn’t worried about the vaccine being harmful to the baby’s development, since the baby’s organs are all well-formed by the third trimester. I was more concerned about the general uncertainty stemming from the fact that pregnant women weren’t included in the vaccine trials. I didn’t want to make a decision that felt unsupported by evidence, so I did my own research.
The CDC and World Health Organization have recently shared new guidance for pregnant women: “Based on what we know about this kind of vaccine, we don’t have any specific reason to believe there will be specific risks that would outweigh the benefits of vaccination for pregnant women.”
I read the Pfizer and Moderna trials published in medical journals, as well as the emergency use memorandums. The memorandums discuss the patients who ended up becoming pregnant during the trial. There have been no adverse pregnancy outcomes in either trial in patients or their fetuses. I also had conversations with my healthcare provider, my husband, who’s an orthopedic trauma surgeon, and co-workers about the risks and benefits.

My doctor said what I hope all OBs are telling their patients: “It’s a case by case decision-making process. You have to weigh your own risks and benefits.”
My mentor, who is also a high-risk OB specialist, told me the same advice that I’ve heard him give many patients who are faced with difficult decisions during pregnancy: “You make a decision with the information you have at the moment. And you don’t look back. Because there’s no such thing as a bad decision when you are making a decision under these circumstances.”
It boiled down to this: What was the risk of my getting COVID in the remainder of my pregnancy? Pregnancy increases the risk for severe illness with COVID, developing respiratory symptoms requiring the ICU, and needing a ventilator, per the CDC.My own risk of exposure was high. I was taking care of COVID-positive patients every day. My husband is also a frontline physician, and my older girls are both in in-person school.
I felt like anything I could do to try to reduce my risk of getting COVID for the remainder of my pregnancy and postpartum would be beneficial for me and for baby—and for my family and patients.
Physically, I felt fine following both doses.
I had a little bit of arm soreness but other than that I had no negative side effects. Neither shot hurt, and I didn’t even feel the second one in the moment.
A lot of people have asked why I didn’t wait until I delivered to get vaccinated. It felt like late pregnancy was the riskiest time for me to potentially get COVID. The end of pregnancy and around the time of delivery are the risky stages of pregnancy because that’s when your body, heart, and lungs have the most stress on them. Those final few weeks of my pregnancy and then immediately postpartum would have been so hard if I had gotten COVID.
And I know that it becomes very stressful logistically for a family to figure out how to best care for everyone when the mom has coronavirus.
When I got the vaccine, it really made me feel like I was doing everything I could to ensure a safe end of pregnancy, delivery, and the postpartum period. That gave me some sense of relief after experiencing a whole pregnancy in a pandemic.
It was wonderful to finally deliver my daughter and have her be here safe and sound.

It was hard to not compare myself to each of my really sick patients throughout my pregnancy. It was hard not to feel helpless at times.
It’s been really nice to turn off my work brain for a little while, be at home, and be a mom and really enjoy these newborn days. The sleepless nights don’t feel quite so bad when you’re coming out of a stressful work environment during a pandemic. I’ll take sleepless nights over that for a little while, at least.
Source: Read Full Article



