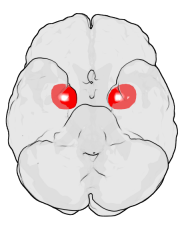
A new study from University of Alberta researchers has shown that traumatic or stressful events in childhood may lead to tiny changes in key brain structures that can now be identified decades later.
The study is the first to show that trauma or maltreatment during a child’s early years—a well-known risk factor for developing mental health conditions such as major depressive disorder in adulthood—triggers changes in specific subregions of the amygdala and the hippocampus.
Once these changes occur, researchers believe the affected regions of the brain may not function as well, potentially increasing the risk of developing mental health disorders as adults during times of stress.
“Now that we can actually identify which specific sub-regions of the amygdala or the hippocampus are permanently altered by incidents of childhood abuse, trauma or mistreatment, we can start to focus on how to mitigate or even potentially reverse these changes,” said Peter Silverstone, interim chair of the Department of Psychiatry and one of a team of eight U of A researchers who conducted the study.
A total of 35 participants with major depressive disorder were recruited for the study, including 12 males and 23 premenopausal females aged 18 to 49 years. Researchers also recruited 35 healthy control subjects, including 12 males and 23 females who were matched by age, sex and education.
“This may help shed some light on how promising new treatments such as psychedelics work, since there is mounting evidence to suggest they may increase nerve regrowth in these areas. Understanding the specific structural and neurochemical brain changes that underlie mental health disorders is a crucial step toward developing potential new treatments for these conditions, which have only increased since the onset of the COVID-19 pandemic,” said Silverstone, who is also a member of the U of A’s Neuroscience and Mental Health Institute.
The study noted that previously “most of the work on the effect of stress on the amygdala and hippocampal substructures has been conducted in animals,” and direct testing of preclinical stress models in humans has been impossible to date. However, “recent advances in high-resolution MRI (magnetic resonance imaging) of the hippocampal subfields and amygdala subnuclei have allowed researchers to test these models in vivo in humans for the first time.”
Once these biological changes occur in stress-related brain structures, researchers say the affected regions of the brain may become “maladaptive” or dysfunctional when people deal with adult stresses, making them “more vulnerable” to developing depression or other psychiatric disorders as adults.
Source: Read Full Article