Countries around the world continue to struggle to contain the coronavirus disease 2019 (COVID-19), despite the development of effective mitigation strategies to reduce the spread of its causative agent, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Recently, thousands of monkeypox cases have been recorded in non-endemic countries. Surveys are underway to determine the source of the infection as well as its transmission routes.
A special report published in Mayo Clinic Proceedings provides an overview of the monkeypox infection, as well as its epidemiology, clinical manifestations, and mitigation strategies in light of the current COVID-19 pandemic.
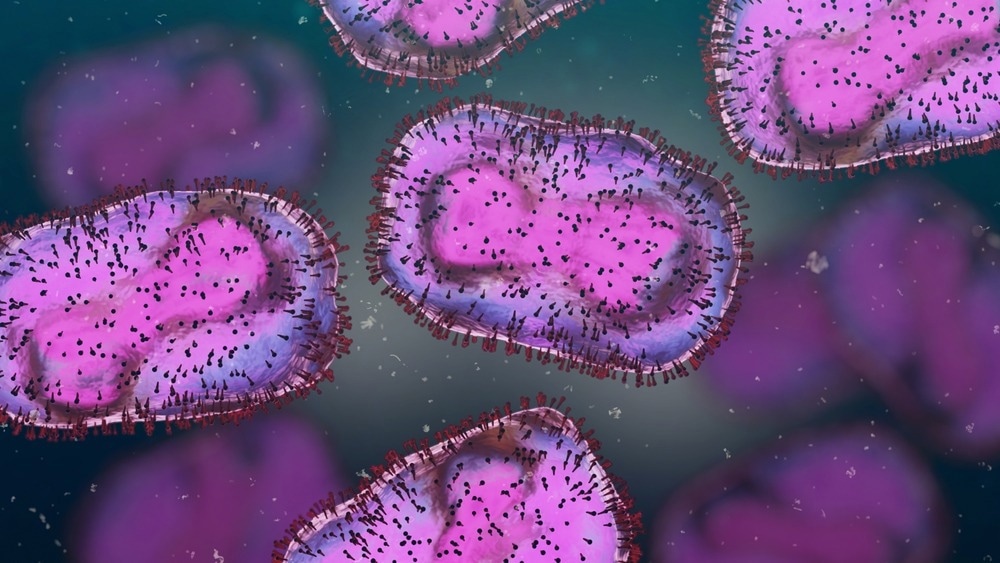
Study: Monkeypox 2022: Gearing Up for Another Potential Public Health Crisis. Image Credit: Dotted Yeti / Shutterstock.com
Virology
The monkeypox virus belongs to the Orthopoxvirus genus of the Poxviridae family. Members of this family have enveloped viruses that consist of double-stranded deoxyribonucleic acid (DNA) genetic material.
The monkeypox virus strains that cause disease in humans can be divided into two clades. These include the West African clade, which is associated with 1-4% mortality, and the Congo Basin (Central African) clade, which has a 10% mortality rate.
The monkeypox virus is less susceptible to mutation than ribonucleic acid (RNA) viruses like SARS-CoV-2. The higher rates of human-to-human transmissions of the monkeypox virus in the current outbreak have raised concerns regarding whether the newer variants have higher transmission capacities.
Epidemiology
In 1970, the first monkeypox infection in humans was identified in the modern Democratic Republic of the Congo. Since then, several Central and Western African countries have reported outbreaks.
The Democratic Republic of Congo reports more than 1,000 monkeypox cases each year. The Central African Republic has reported 19 cases, whereas Nigeria is combatting an active and ongoing outbreak that includes over 80 cases.
An isolated outbreak of monkeypox was documented in the United States in 2003, which was caused by prairie dogs that became sick after being housed with imported rodents from Ghana. Before the current outbreak, the monkeypox virus was also detected in Singapore, Israel, and the United Kingdom.
Clinical features
Generally, the symptoms of monkeypox infection will develop within 6 to 13 days following infection; however, it has been associated with an incubation period of up to 21 days.
According to the World Health Organization (WHO), monkeypox infection can be classified into two phases. The initial invasive phase typically lasts about five days and is characterized by fever, lymphadenopathy, headache, myalgia, malaise, and asthenia.
Subsequently, the skin eruption phase occurs one to three days after the fever has begun. This phase is characterized by macules and papules on the face and trunk, which gradually evolve into vesicular and pustular rashes by the seventh day. Eventually, the rash spreads to the palms and soles of the feet.
The disease caused by the monkeypox virus typically resolves between two and four weeks following the initial infection. However, children, pregnant women, and other immunocompromised patients may experience a more severe form of the disease.
Diagnosis
Skin/crust from the surface or a swab taken from infected lesions are appropriate specimens for diagnosis. These samples are subsequently tested through the polymerase chain reaction (PCR) assay.
Electron microscopy can reveal a pox virus in skin lesion samples; however, this technique is not typically used for diagnostic purposes.
Due to the cross-reactivity between orthopoxviruses and the possibility of false-positive results in individuals who have previously received a smallpox vaccine, serological testing is not advised.
Infection control measures
Monkeypox transmission primarily occurs through direct contact with an infected individual or material or through exposure to respiratory droplets from an infected person. As a result, several measures can be taken to reduce an individual’s risk of infection.
Some contact precautions include the use of gowns and gloves, whereas droplet precautions can involve the use of protective eyewear. Conversely, airborne precautions include the placement of a patient in a negative air room with adequate air exchanges, combined with the use of an N-95 respirator or higher respiratory protection.
Taken together, each of these precautionary measures has been recommended by the United States Centers for Disease Control and Prevention (CDC) when monkeypox is suspected. Since monkeypox cases are currently restricted to individuals who have direct contact with known cases, obtaining a detailed history of a suspected case is essential.
Treatment
The primary treatment for monkeypox infection should be symptom-focused and supportive. Clinicians must also be vigilant for secondary bacterial infections and, as a result, should initiate appropriate direct antibiotic therapy as needed.
Tecovirimat, which is an antiviral medication that inhibits the major envelope protein of the orthopoxvirus, has been found to protect non-human primates against monkeypox infection. Similarly, cidofovir and brincidofovir have also demonstrated effective antiviral activity against the monkeypox virus in non-human primates.
Postexposure management
Smallpox vaccination is believed to prevent monkeypox infection in those suspected of being exposed to the disease, as the incubation period is relatively long. During orthopoxvirus outbreaks, "ring vaccination" is used to immunize those with previous contact with confirmed cases.
The ACAM2000 vaccine protects against diseases caused by orthopoxviruses, such as smallpox and monkeypox. Since ACAM2000 is a live virus vaccine, it cannot be used in immunocompromised individuals.
Conversely, the JYNNEOS vaccine, which is also known as Imvamune or Imvanex, confers immunity against orthopoxviruses and is safe for immunocompromised patients. Vaccinia immunoglobulin (Ig) is currently being investigated for postexposure prophylaxis in highly immunocompromised patients.
- Ranganath, N., Tosh, P., O’Horo, J., et al. (2022). Monkeypox 2022: Gearing Up for Another Potential Public Health Crisis. Mayo Clinic Proceedings. Doi:10.1016/j.mayocp.2022.07.011
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Antibiotic, Assay, Children, Coronavirus, covid-19, Diagnostic, DNA, Electron, Electron Microscopy, Epidemiology, Fever, Genetic, Headache, immunity, Immunoglobulin, Infection Control, Lymphadenopathy, Microscopy, Monkeypox, Mortality, Mutation, Pandemic, Polymerase, Polymerase Chain Reaction, Prophylaxis, Protein, Public Health, Rash, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Skin, Smallpox, Syndrome, Vaccine, Virology, Virus

Written by
Nidhi Saha
I am a medical content writer and editor. My interests lie in public health awareness and medical communication. I have worked as a clinical dentist and as a consultant research writer in an Indian medical publishing house. It is my constant endeavor is to update knowledge on newer treatment modalities relating to various medical fields. I have also aided in proofreading and publication of manuscripts in accredited medical journals. I like to sketch, read and listen to music in my leisure time.
Source: Read Full Article