The annual meeting of the American College of Allergy, Asthma & Immunology was held virtually this year from Nov. 12 to 16 and attracted participants from around the world, including allergy and immunology specialists as well as other health care professionals. The conference featured presentations focusing on the latest advances in the prevention and treatment of asthma, food and medication allergies, immune dysfunction, and sleep apnea.
In a prospective, multicenter cohort study, Dannielle Brown, of the Northwestern University Feinberg School of Medicine in Chicago, and colleagues found that nearly one in five school-aged children have ever been bullied due to their food allergy.
The authors evaluated food allergy-related racial differences among Black and White children, 12 years of age or younger at study enrollment, with an allergist-diagnosed immunoglobulin E-mediated food allergy. The researchers observed no significant racial differences in food allergy-related bullying prevalence; however, Black children experienced bullying for reasons other than food allergy twice as frequently as White children. In addition, the majority of parents who knew their child was being bullied and did something to stop the bullying reported that their intervention was helpful.
“Food allergy-related bullying among school-aged children does exist; therefore, increasing both school policy awareness for parents and educational food allergy awareness for parents and other students is important in reducing the incidence of bullying,” Brown said. “Clinicians (whether primary care or allergists) could take a few minutes to screen patients with food allergy for bullying during routine appointments by using open-ended questions about patient experiences to gather information without specifically labeling their experiences as bullying.”
Press Release
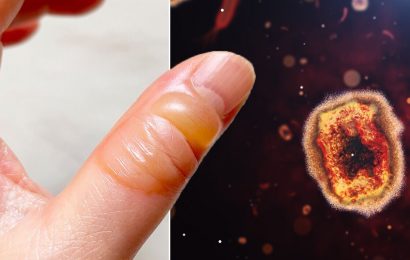
In a case report, Yashu Dhamija, M.D., of the University of Cincinnati College of Medicine, and colleagues identified a patient experiencing contact dermatitis on their face due to the use of a face mask to protect against COVID-19 infection.
Dhamija discussed the case report of a 60-year-old Black man with adult-onset eczema, contact dermatitis, and chronic nasal allergies treated in their clinic after he was seen in the emergency department multiple times for a facial rash. Dhamija and the clinic surmised from all available emergency department information and presentation in the clinic that the patient’s facial rash was likely tied to the use of a face mask. The patient’s condition developed in April 2020, when the patient started wearing a face mask because of the COVID-19 pandemic. Dhamija and his clinical team noted that the patient’s facial rash was where the elastic part of the mask touched the face (likely because of a rubber allergy). Based on this information, Dhamija and his clinical team changed the patient’s medication and advised the patient to wear a cotton-based, dye-free mask without elastic.
“It is important for providers to recognize this problem in patients. There is a benefit in protecting patients from COVID-19 infection by wearing masks and we can offer solutions,” Dhamija said. “In cases of sensitization to rubber components, we recommend patients make a mask at home using U.S. Centers of Disease Control and Prevention guidelines, but without elastic components. Patients can also be instructed to call manufacturers to verify a lack of sensitizers in products, whether they are struggling with face masks or personal care products.”
Press Release
Jonathan Silverberg, M.D., Ph.D., of the George Washington University School of Medicine and Health Sciences in Washington, D.C., and colleagues identified considerable racial and ethnic disparities in childhood atopic dermatitis.
The authors evaluated data from multiple studies that examined health outcomes in U.S. children and adults, including U.S. population-based cross-sectional surveys (National Survey of Children’s Health, Atopic Dermatitis in America study, Medical Expenditure Survey, National Health Interview Survey), longitudinal surveys (The Fragile Families and Child Wellbeing Study), nationwide studies of U.S. hospitalizations (Nationwide Inpatient Sample), and emergency department visits (Nationwide Emergency Department Sample). The researchers found that compared with White children, Black children in the United States had higher rates of atopic dermatitis, more persistent childhood atopic dermatitis, and more nights of sleep loss. In addition, Black and Hispanic children had more severe atopic dermatitis and poorer overall health than White children.
“Black and Hispanic children with atopic dermatitis had lower household income, were more likely to be uninsured or underinsured, and reported insufficient time during the patient-physician encounter,” Silverberg said. “Lower income and lack of private insurance do not account for all of the racial/ethnic disparities observed in atopic dermatitis. Multiple interventions are needed to eliminate these disparities.”
Press Release
In a retrospective chart review, Dylan Timberlake, M.D., of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues found that asthma and/or atopic disease were not associated with any significant increased risk for severe disease related to COVID-19 infection.
The authors evaluated the charts of all patients admitted to Nationwide Children’s Hospital and The Ohio State University Wexner Medical Center in Columbus who had a positive polymerase chain reaction test for severe acute respiratory syndrome coronavirus 2. The charts were reviewed for data on documentation of asthma or atopic disease, defined as asthma, allergic rhinitis, atopic dermatitis/eczema, or food allergy, as well as pertinent comorbidities such as age, gender, and chronic obstructive pulmonary disease. Rates of intensive care unit admission, supplemental oxygen requirement, intubation, and mortality were compared for patients with versus without asthma and for atopic patients versus nonatopic patients. The researchers found that neither asthma nor atopic disease appeared to be associated with increased or decreased severity of COVID-19 infection.
“We did notice a trend towards decreased odds of mortality for patients with atopic disease and COVID-19 (P = 0.16), but this did not reach statistical significance,” Timberlake said. “While there are obvious limitations to a retrospective chart review, this study accompanied with other recent studies continues to show that neither asthma nor atopic disease are associated with severe disease with COVID-19.”
Press Release
Source: Read Full Article