Hokkaido University researchers have analyzed the suitability of a smooth, flexible and transparent material used to make model arteries for use in medical teaching and surgical training. Their work is described in the Journal of Vascular and Interventional Radiology.
Ever-improving 3D printing technology can create models of blood vessels that are significantly more realistic than those made with more conventional methods, and they are also much more suitable for surgical practice than virtual simulations. All types of models and simulations are applied in two key situations. They assist in medical education, allowing students of general medicine and of surgery to learn how to handle and manipulate blood vessels before applying their skills on patients. The sophistication of 3D printing also allows highly accurate models of an individual patient’s artery and vein structure to be built from radiology scans, allowing surgeons to practice on a model before performing complex surgery.
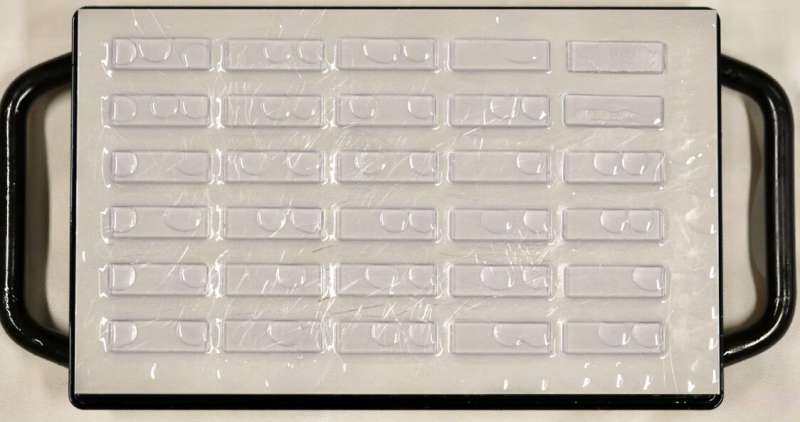
The Hokkaido team has improved assessments of the 3D printing technology by studying a material used to make model arteries that are transparent to allow careful inspection while recreating the flexibility, smoothness and slipperiness of real arteries. They tested the accuracy and suitability of the modeling materials by comparing their properties with pig arteries, measuring parameters including adhesive and tensile strength, compressibility and friction characteristics.
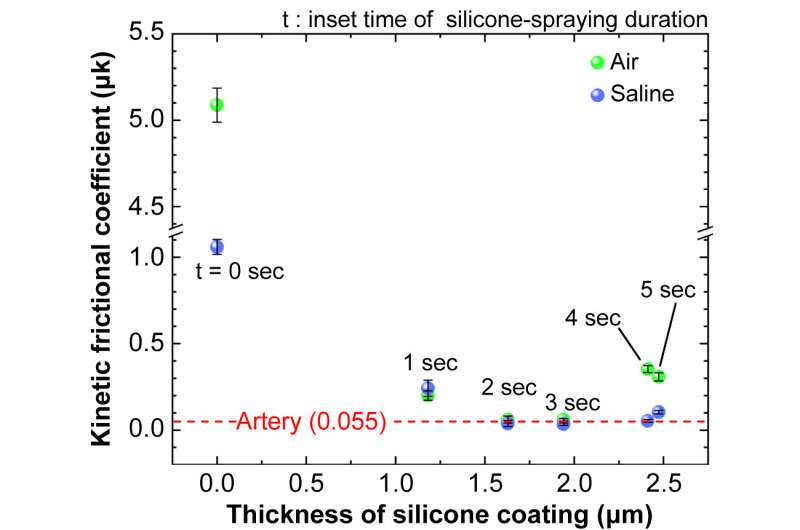
“We hypothesized that a tailored 3D modeling material called Flexible 80A resin would effectively simulate the properties of real arteries,” says interventional radiologist Ryo Morita of the Hokkaido research group. “Our studies confirmed the material’s suitability, while at the same time identifying differences between the model material and the pig arteries that could guide further improvements.”
The researchers point out that future research will be needed to address some limitations of this early work. Moving on to use real human arteries for comparison would improve the relevance for working on patients. The methods used in this initial study could also be applied to a variety of other modeling resins to identify those most suitable. They would also like to investigate how differences they identified in tensile strength between the models and the pig arteries might affect the use of the models by physicians.
While creating custom models for an individual patient can be of great assistance in preparing for surgery, it is expensive and time-consuming. This limits the use of personalized models to only the most anatomically challenging cases. “Making and storing models made with improved 3D printing processes could build a bank of examples for use in preoperative planning and for training,” Morita concludes.
More information:
Ryo Morita et al, Mechanical Properties of a 3 Dimensional–Printed Transparent Flexible Resin Used for Vascular Model Simulation Compared with Those of Porcine Arteries, Journal of Vascular and Interventional Radiology (2023). DOI: 10.1016/j.jvir.2023.01.008
Journal information:
Journal of Vascular and Interventional Radiology
Source: Read Full Article


