A new Nature Immunology study led by University of Pittsburgh and National Institutes of Health researchers sheds light on how a rare type of helper T cell, called Th9, can drive allergic disease, suggesting new precision medicine approaches to treating allergies in patients with high levels of Th9.
“Th9 cells are kind of like the black sheep of helper T cells,” said senior author Daniella Schwartz, M.D., assistant professor of rheumatology at Pitt’s School of Medicine. “They need a perfect storm of occurrences to pop up, and they aren’t long-lived, which makes them hard to study. The other weird thing about Th9 cells is that they remain functional without seeing their antigen.”
T cells switch on when they encounter viruses, bacteria or other pathogens, causing them to ramp up production of inflammatory proteins called cytokines, which control a suite of immune responses via the JAK-STAT signaling pathway. The main “on” switch for T cells is when the T cell receptor recognizes an antigen, a specific identifying feature of a threat. Beyond this specific form of activation, there’s also another type of switch known as bystander activation, which doesn’t involve the T cell receptor.
“Bystander activation usually requires other types of dangerous signals that indicate a threat,” said Schwartz. “What’s really unusual about Th9 cells is that they can be turned on even without these dangerous signals.”
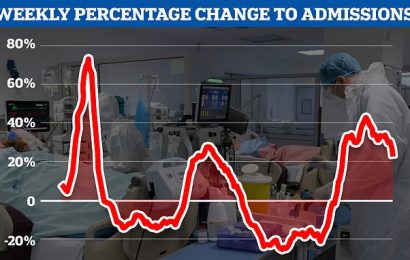
To learn more about how Th9 cells are activated in allergic responses, Schwartz and her team measured IL9, a cytokine produced by Th9 cells, in T cells from patients with atopic dermatitis, an allergic condition characterized by a dry, itchy rash, and healthy volunteers. They found that Th9 cells from the allergy patients responded to bystander activation, but not those from healthy volunteers.
“This told us that there’s some sort of checkpoint that prevents non-specific activation of Th9 cells in healthy people,” explained Schwartz. “In allergy patients, we hypothesized that the checkpoint breaks down, so you’re getting production of the cytokine even without restimulating the cells with antigen.”
In most helper T cells, when antigen binds to T cell receptor, this highly specific recognition process causes DNA in the T cell’s nucleus to unwind like thread on a spool, opening up regions of DNA that encode the production of cytokines that unleash a suite of immune responses. When the threat is eliminated, there’s no more antigen to stimulate T cell receptors and the cells turn off. But the DNA structure remains open so that the cell is poised for a possible future encounter.
Schwartz and her team found that Th9 cells have a different type of regulation. These cells are activated by transcription factors called STAT5 and STAT6, which bind to the open region DNA around IL9 to activate the gene. Unusually, the DNA closes over time, shutting down production of IL9.
In healthy people, this opening and closing mechanism acts like a checkpoint to manage immune responses being on all the time. But when this checkpoint breaks down in allergy, the DNA remains open, keeping the IL9 gene switched on and driving allergic inflammation.
In a mouse model of allergic asthma driven by Th9, blocking JAK-STAT signaling with a drug called tofacitinib, which is approved for treating rheumatoid arthritis, atopic dermatitis and other inflammatory disorders, improved disease symptoms
Analyzing data from allergic asthma patients, the researchers found that those with higher levels of Th9 cells had greater activation of STAT5 and STAT6-related genes. This finding supports the idea that Th9 could act as a biomarker to predict patients who are likely to respond to JAK inhibitors, pointing to new approaches for allergy precision medicine.
More information:
Aran Son et al, Dynamic chromatin accessibility licenses STAT5- and STAT6-dependent innate-like function of TH9 cells to promote allergic inflammation, Nature Immunology (2023). DOI: 10.1038/s41590-023-01501-5
Journal information:
Nature Immunology
Source: Read Full Article