Child and adolescent mortality rates in the United States rose by 20% between 2019 and 2021, the largest increase in at least 50 years, according to an editorial published Monday in the Journal of the American Medical Association. These increases follow decades of progress in lowering the rate of death from childhood diseases. The alarming spike in pediatric mortality is primarily due to deaths from homicide, accidental drug overdoses, motor vehicle accidents and suicide among those ages 10 to 19.
The new research is based on a detailed examination of death certificate data from the Centers for Disease Control and Prevention. The analysis revealed that the mortality rate of Americans ages 1 to 19 rose by 11% between 2019 and 2020 and an additional 8% between 2020 and 2021.
“I have not seen this in my career,” said lead author Steven Woolf, M.D., director emeritus of the Center on Society and Health at Virginia Commonwealth University.
“For decades, the overall death rate among U.S. children has fallen steadily, thanks to breakthroughs in prevention and treatment of diseases like premature births, pediatric cancer and birth defects. We now see a dramatic reversal of this trajectory, meaning that our children are now less likely to reach adulthood. This is a red flashing light. We need to understand the causes and address them immediately to protect our children.”
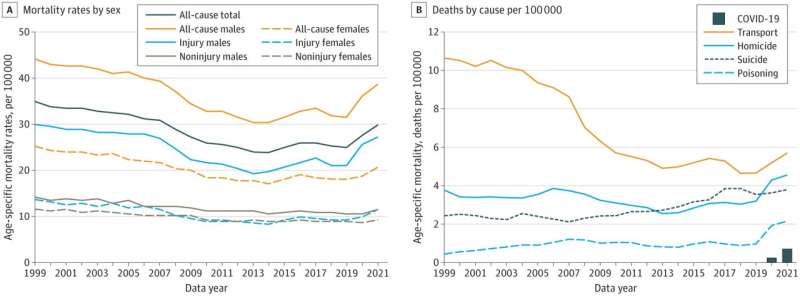
The recent increase in “all-cause mortality,” a measure of all deaths in children and teens, is largely driven by increases in certain injury-related deaths, which began well before the COVID-19 pandemic. For example, the researchers found that suicide rates at ages 10-19 began increasing in 2007 and climbed by 70% by 2019. Homicide rates began increasing in 2013, rising by 33% by 2019. The number of overdose deaths began to rise in 2019, and deaths from car accidents dramatically jumped in frequency in 2020 and 2021.
“We’ve now reached a tipping point where the number of injury-related deaths is so high that it is offsetting many of the gains we’ve made in treating other diseases,” said Elizabeth Wolf, M.D., an assistant professor in the Department of Pediatrics at the VCU School of Medicine and pediatrician at the Children’s Hospital of Richmond at VCU.
In addition to Woolf and Wolf, the study was co-authored by Frederick Rivara, M.D., a professor of pediatrics at the University of Washington and Seattle Children’s Research Institute and acclaimed expert on pediatric injury prevention.
While deaths from COVID-19 contributed to the recent increase in child mortality, its impact was overshadowed by the increase in deaths from injuries, according to the data. In 2020, the mortality rate from COVID-19 among children and adolescents was 0.24 deaths per 100,000, whereas the increase in injury-related deaths alone was nearly 12 times higher.
“A large proportion of these deaths involve firearms, the method most commonly used by teens to die by suicide or commit homicides. Firearm ownership has increased, guns are more available to young people, and the weapons are more lethal,” said Woolf, a professor in the Department of Family Medicine and Population Health at the VCU School of Medicine.
“Mass shootings at schools receive a lot of national attention, but what adds up to a much larger death toll are the shootings of children, one by one, that we hear about on our local nightly news.”
Another major driver for these trends is the worsening mental health crisis affecting young people, Wolf said.
“There is a severe shortage of mental health providers who care for children and adolescents, especially in rural areas,” she said. “It’s estimated that only half of children with a treatable mental health condition have access to a mental health professional.”
Although the pandemic did not initiate these trends, it may have poured fuel on the fire, the researchers said.
“Children and teens were impacted by the pandemic in so many indirect ways, whether from the death of a caregiver or extended school closings,” Wolf said. “The pandemic also upended health care delivery, making it harder for children to attend routine checkups and receive important vaccinations.”
The risk of injury-related death also varied significantly by race and ethnicity. In 2021, Black youths ages 10-19 were 20 times more likely to die by homicide than white and Asian American/Pacific Islander youths and six times more likely than Hispanic youths. Death by suicide was more than twice as likely among Black and American Indian/Alaska Native youths than white youths. American Indian/Alaska Native youths faced the greatest risk of dying in a motor vehicle accident.
“These disparities have a history. They reflect the social and health consequences of policies that, for generations, have marginalized people of color, segregated neighborhoods, and choked off resources for economic development,” Woolf said. “The legacy of this history is that communities of color are at much higher risk of economic stress and social conflict.”
Without bold research and policy actions to reverse the trend, children’s risk of not reaching adulthood may continue to increase, according to the researchers.
“The need to address policies on firearms and mental health is obvious, but we must also address the root causes of these deaths by expanding opportunities for education, well-paying jobs, good housing, and other living conditions. More research is also needed to better understand and address the increase in injury deaths,” Woolf said.
“Modern medicine has fought the battle against pediatric diseases, but the threats to our children are now manmade. Without action, bullets, drugs and automobiles will continue to claim the lives of our most cherished population.”
More information:
Steven H. Woolf et al, The New Crisis of Increasing All-Cause Mortality in US Children and Adolescents, JAMA (2023). DOI: 10.1001/jama.2023.3517
Journal information:
Journal of the American Medical Association
Source: Read Full Article


