Depression sucked the life from Lori Jackson’s time on this earth for nearly 40 years. On her darkest days in college she hung a blanket over her dorm room window to block out the light and slept, skipping classes.
As she had her three children, her doctor prescribed Prozac for postpartum depression, but that didn’t lift the darkness.
“It’s hard to describe, and it’s kinda cliche maybe. … You just feel like somebody has put a black, non-see-through blanket over your head,” said Jackson, who is 55 and lives in Overland Park, Kansas. “It’s heavy and it’s black and it’s just always there. You really can’t comprehend it unless you’ve experienced it.”
She tried so many unsuccessful depression treatments—including electroconvulsive therapy at a Johnson County hospital—she didn’t care whether she lived or died by the time her Kansas City psychiatrist, Dr. Irfan Handoo, asked her to try just one more thing.
It was something he was excited about, a newer version of TMS—transcranial magnetic stimulation—a non-invasive therapy he and other psychiatrists have used for years to treat major depressive disorder.
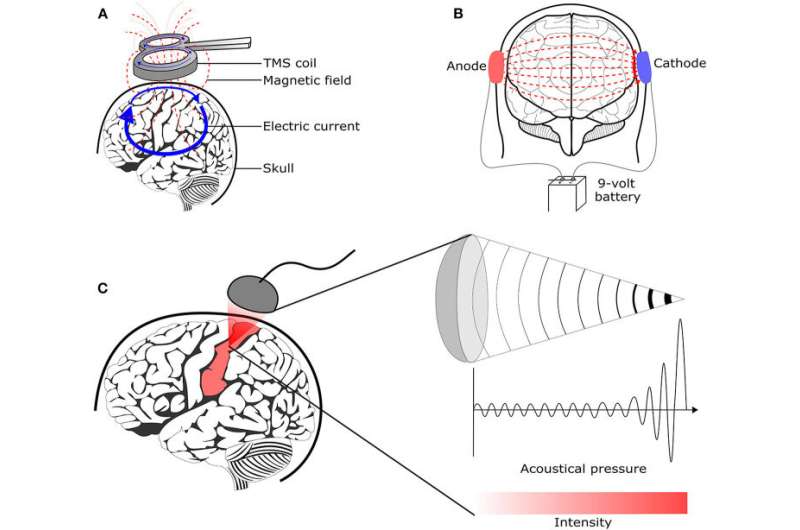
With TMS, approved by the U.S. Food and Drug Administration in 2008, patients wear an electromagnetic coil on their head. It creates a magnetic field, sending electric pulses through their skull and stimulating nerve cells in a part of the brain involved in regulating mood.
Handoo wanted Jackson to try a newer version of the therapy called Deep TMS that delivers those pulses even deeper into the brain. It is approved by the FDA for patients who aren’t getting better by taking antidepressant medications.
Handoo is among the first and one of the few psychiatrists offering Deep TMS therapy in the Kansas City area.
“When I saw Lori, she had one of the most severe cases of depression I’d seen,” Handoo told The Star. “She was having active suicidal thoughts on almost a daily basis. And she had given up.
“But I said do not give up. I said I’m telling you I’ve done the research, just believe me. We’re going to do something that’s far better. And to her credit she believed me.”
It changed her life.
Jackson, on a recent weekday afternoon, sat in an exam room in Handoo’s Kansas City office with what looked like an oversized bicycle helmet on her head, hooked up to a machine behind her.
When the 19-minute treatment began, a burst of jackhammer noise exploded into the room.
Rat-a-tat-tat. Rat-a-tat-tat. Rat-a-tat-tat.. Rat-a-tat-tat.
Under the padded helmet, the corners of Jackson’s eyes twitched. Her jaw involuntarily clenched. Some patients wear a mouth guard but she did not. She did, though, wear earplugs.
Rat-a-tat-tat. Rat-a-tat-tat. Rat-a-tat-tat. Rat-a-tat-tat.
She said later the pulses—delivered in a 2-seconds-on-20-seconds-off rhythm—are an odd sensation, but not painful.
“It’s completely doable,” she said.
And for the first time in nearly 30 years, Jackson’s depression has lifted.
For the first time in nearly 30 years, she’s holding down a job, as an office assistant. Depression is a leading cause of disability worldwide, the World Health Organization says.
“The sun is shining, it really is,” she said. “And the blanket’s gone. I don’t feel any depression. Now, there’s things … I feel discouraged about that. Note that I didn’t say I feel depressed about that, which normally would have set me in a hole.
“It’s miraculous, the way I feel. My brain did a complete 180.”
About 1 in 5 people will experience depression in their lifetime, and it is treatable for most. But some estimates suggest as many as 40% of patients are considered treatment-resistant like Jackson. And at some point, some of them give up trying and simply live in the dark.
But that’s not happening in Handoo’s office, which bought a Deep TMS machine created by international medical technology company BrainsWay. Since Dec. 1, Handoo has been administering the therapy to about 20 patients a day.
Most insurance plans will cover deep TMS treatments, Handoo said.
“It certainly is a new advance because it does go deeper into the brain and can do things other TMS coils cannot,” said Dr. Mark George, a professor of psychiatry, neurology and radiology at the Medical University of South Carolina in Charleston.
George is recognized as a pioneer of TMS therapy and has written that brain stimulation methods have progressed “from unusual novelties and way-out ideas to sophisticated treatments that are now saving lives daily.”
George has worked with TMS for nearly 30 years and “the progress in my lifetime has been truly amazing,” he said.
“Now it’s a mainstream treatment, which is wonderful. I mean it really is good that there are millions of people on planet Earth now who are not depressed and living better lives because of the technology that’s relatively safe and side effect free.”
How does TMS work?
Before Handoo suggested she try this newer version of TMS, Jackson came up empty with just about every method used to treat depression. ECT (electroconvulsive therapy). IV ketamine treatments used to treat major depression. She had tried traditional TMS, too, with no benefit. And, 30 different medications.
Handoo couldn’t blame her for feeling hopeless.
“All studies show that when it comes to treatment-resistant depression, once somebody’s tried and failed to respond to four or more different anti-depressants, the chance of anti-depressant No. 5 or No. 6 being that magic bullet starts to decrease with every successive medication failure,” Handoo said. “Medications can only do so much.”
Researchers say brain stimulation methods are not meant to compete with medications or traditional talk therapy, and in some cases have been found to be more effective when used with other therapy.
And yet, they say, as depression and suicide rates increase, many patients don’t know much about TMS—described as a tickling of the brain.
One estimate suggests that less than 5% of patients with depression who are eligible to receive the therapy actually get it.
The University of Kansas Health System has offered TMS therapy for the last few years, said Dr. Tyler Kjorvestad, a psychiatrist and internal medicine doctor who leads the comprehensive depression assessment and treatment clinic there.
During TMS therapy, a magnetic field targets the “dorsal lateral prefrontal cortex,” he said, an area that isn’t as active in patients with depression.
“We know that magnetic or electric stimulation of this area can actually increase the neural activity of that area. So basically we’re turning on or turning up a part of the brain that’s not necessarily always active in people with depression.”
The magnetic pulses from traditional TMS, Handoo said, travel 0.7 centimeters into the brain, where Deep TMS, using a different configuration of coils, can reach 4 to 5 centimeters and stimulates deeper and wider regions. (Because of the pulsing, this therapy is known as rTMS, repetitive transcranial magnetic stimulation.)
Handoo said a TMS machine runs about $60,000; a deep TMS machine costs about $250,000.
BrainsWay, the maker of the Deep TMS machine Handoo uses, “has done a lot of good research where they’ve investigated using it for treatment of other conditions, not just depression,” said George. “And they’ve recently gotten (FDA) approval as well to use it for people who want to stop smoking.”
George, who works with veterans at a VA hospital, said studies are ongoing about whether TMS therapy is effective in treating post-traumatic stress disorder.
“In terms of looking at the future, I think there will be more and more brain conditions where we understand the circuitry and then we can use TMS to modify it,” said George. “Right now we have about four diseases that can be treated with TMS and I wouldn’t be surprised in a couple of years from now we have 10 or 12.”
‘It just stings a little bit’
Handoo’s lead TMS technician, Stefanie Sizemore, jokes with patients that they’re suiting up for a biathalon because during the sessions they wear a tight-fitting cap, like a swim cap, under a helmet.
“It just stings a little bit,” said Jackson. “It’s not painful. If it is, they just move the helmet.”
A 2019 study in the Journal of Psychiatric Research that caught Handoo’s attention concluded that Deep TMS, used with standard antidepressants, is significantly more effective at reducing depression in patients with major depressive order than standard TMS or medication-only treatment.
But both methods of TMS, used with medication, were more effective than drugs alone for the nearly 230 study participants with treatment-resistant depression, researchers found.
Sessions of traditional TMS can typically last 40 minutes. Deep TMS sessions are 19 minutes. “So patients can get in and out of here,” said Handoo, who has a TV set up on the wall opposite the treatment chair so patients can Netflix and chill.
The sessions are short, but there are many, which George said can be an obstacle for people who don’t live close to a treatment center. Patients have to come every day, weekends off, for six weeks in a row. The session Jackson allowed The Star to watch was her 32nd.
She completed the last of 36 sessions on July 29.
“It takes time, it’s a little loud, it’s a little uncomfortable,” said George. “But over my 30 years I’ve seen just a handful of people who were unable to tolerate a treatment or have given up. Most people say if this is what it takes to get my depression better, bring it on.”
Many times it can take up to two months after the last treatment to feel the full benefits, said Handoo.
During their treatment he monitors patients’ progress with the PHQ-9, a depression rating scale used worldwide. Jackson began therapy at the high end of 24, indicating severe depression—and had improved to a 6 as of her last treatment in July.
“it’s a dramatic improvement,” said Handoo.
There’s also a difference that can’t be measured. When she first came to him, Jackson wore the flat, emotionless facial expression of a person trapped in depression. Today, she can muster a smile.
“Just like medications that take weeks to work, TMS doesn’t work immediately after that first treatment,” Kjorvestad at KU said. “It takes a week, two weeks, three weeks, four weeks sometimes, for those structural changes in your brain to occur so that you start engaging with the environment differently.”
One drawback to TMS, George said, is that doctors don’t know at the outset whether a patient will respond.
“So the biggest complaint that sticks with me as a provider, people come and they sit in the chair for 30 sessions and … about a third of people won’t get better. So that’s a big complaint, that they’ve gotten their hopes up and have done all this work and they’re no better,” said George, joking that a Harry Potter sorting hat would be helpful.
But Kjorvestad has seen TMS therapy open up new worlds for patients, from allowing them to return to work like Jackson to improving personal relationships. He has seen older patients blossom, patients in their 70s, 80s who could not tolerate anti-depressants.
“When you can give a patient the option to have a treatment like this that doesn’t require them to take a daily medication, or interfere with the other medications they might be on, it’s really a great option to give them their life back,” he said.
“Especially if before they were really isolated, they couldn’t get out and spend time with their friends and family. Because that really does happen a lot in that population. Those are the most rewarding patients for me.”
It’s not shock therapy
Jackson’s mother suffered from depression, too. “She was high-functioning depression,” Jackson said. “I succumbed to it and I shut down and couldn’t function. But my mom was supermom. We had a home meal every day. I was the exact opposite.”
As an adult, short bouts of depression that “would pass” eventually became longer and longer. Jackson didn’t realize she needed professional help until after she had her second child in 1995. “The pregnancy really kicked it in and it just snowballed,” she said.
More than 10 years ago, before she was Handoo’s patient, Jackson had shock therapy as her marriage crumbled and her depression deepened. “My brain is still messed up. It caused short-term memory problems,” she said.
TMS is not ECT, or what some people call shock therapy. During that procedure a patient is given anesthesia in a hospital and seizures are induced.
ECT is a “lifesaver” for some patients, said George. “But it’s a whole different level of side effects and potential risks.”
It can cause severe long-term and short-term memory issues that can last for years, as Jackson’s did, said Handoo, who said Deep TMS is the only thing he’s seen that has helped resolve some of those short-term memory problems caused by ECT.
During her TMS treatment session, Jackson told Handoo that she had already noticed her memory improving.
“You’re already noticing that?” Handoo said.
“Yeah,” she said.
“Wow, that’s shocking,” said Handoo.
A “very rare” side effect of TMS, George said, happens when the brain is stimulated too long and too fast, which can cause accidental seizure.
“The good news is that when those happen they happen while you’re in the chair, with the nurse right beside you, they stop on their own, and no one has gone on to have recurrent seizures or epilepsy or any kind of problems with that,” said George.
It can be difficult to encourage people with depression to seek professional care, but having many and varied methods of therapy, other than taking a pill, can help, said Kjorvestad.
Source: Read Full Article