Scientists at the University of Illinois Chicago have found new evidence that people with severe COVID-19 may have something in common: an early and persistent activation of neutrophils, a type of white blood cells that the immune system uses to fight bacteria.
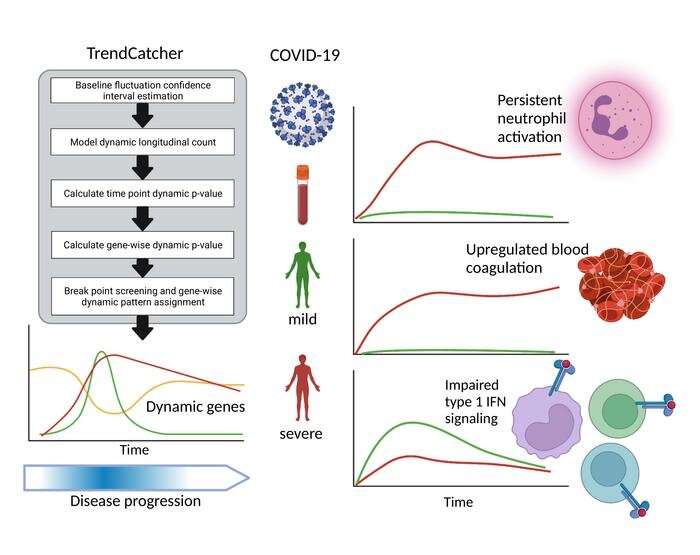
They made this observation after first building and validating a computational model to identify trends in gene expression over time and then applying it to datasets of SARS-CoV-2 infection in animals and people. The research team leveraged the model—called TrendCatcher—to better understand at what point during an infection are genes of the immune cells circulating in blood turned on or off.
“Studying changes in gene expression over the course of a disease can provide important information about the biological mechanisms that differentiate between people with mild and severe illnesses,” said the lead author Dr. Jalees Rehman, professor in the department of pharmacology and regenerative medicine and the department of medicine at the UIC College of Medicine. “This can give researchers many clues to develop effective treatments that target specific cells early on in the disease.”
The study’s first author is Xinge Wang, a UIC Ph.D. student in the department of biomedical engineering. Wang developed the TrendCatcher software to identify trends in gene expression data obtained from a broad range of patients, including those who developed only mild symptoms as well as those who had severe disease.
Identifying the gene signatures, which are linked to developing severe COVID-19, early on in the disease also would allow health care providers to start treating high-risk patients with the necessary medications even before the disease progresses.
For their experiments, the team analyzed publicly available gene expression data from blood samples collected from patients as soon as they were diagnosed with SARS-CoV-2 infection as well as in the subsequent weeks. The researchers found the early and persistent activation of neutrophils was a hallmark of patients who progressed to severe COVID-19. Activation of neutrophils occurred within the first week after the initial diagnosis and persisted for approximately four weeks in patients who developed COVID-19. In some severe COVID-19 patients, neutrophils remained active for up to six or seven weeks. Patients with mild COVID-19 showed minimal neutrophil activation.
The researchers also found that healthy immune responses included upregulation of interferon protein signaling, an antiviral defense mechanism of the human body. Patients with mild COVID-19 showed early activation of the interferon pathway, similar to what was seen in individuals receiving a SARS-CoV-2 mRNA vaccination.
Their study, titled “Temporal transcriptomic analysis using TrendCatcher identifies early and persistent neutrophil activation in severe COVID-19,” is published in the journal JCI Insight.
“The findings reported in this study could potentially form the basis of developing or delivering COVID-19 therapies that are appropriate for a given time window,” Rehman said. “Because we know that neutrophil activation is associated with severe COVID-19 illness, further validation of these findings could lead to a simple blood test at key windows of time to indicate a patient should be prioritized for available treatments.”
Rehman said that this evidence also helps to support other studies that suggest excessive neutrophil activation may explain why some patients develop severe COVID-19 whereas others do not.
“Specifically treating excessive neutrophil activation would prevent damage to the body’s own tissues by suppressing hyperactive neutrophils while allowing other immune cells to do their job and eliminate the virus,” Rehman said.
Source: Read Full Article


