Survivors of extracorporeal membrane oxygenation (ECMO) life support had a 24% higher rate of new mental health diagnoses after discharge compared to other ICU survivors, according to the first study of its kind, published in JAMA.
ECMO, or extracorporeal membrane oxygenation, is the most advanced form of life support. It temporarily replaces the heart and lungs of patients suffering from heart or respiratory failure. This resource-intensive treatment is usually reserved for younger, healthier patients who are most likely to survive. This is the first study to look at how their mental health is affected.
“ECMO saves lives. About 50 to 65% of patients who receive this treatment will survive, and most are alive five years later,” said Dr. Shannon Fernando, a critical care physician at Lakeridge Health and postdoctoral fellow at The Ottawa Hospital and the University of Ottawa.
“We already knew that ICU survivors can suffer mental health impacts from the trauma of invasive treatments, living with new physical limitations and dealing with long recovery times. We suspected ECMO survivors would be at greater risk of mental health impacts because they are sedated and ventilated for longer and often face a more challenging recovery. But we didn’t have clear data until now.”
To find out, the team of researchers from The Ottawa Hospital, the Institut du Savoir Montfort, ICES and the University of Ottawa looked at health records from all ICU survivors in Ontario, Canada from April 2010 to March 2020.
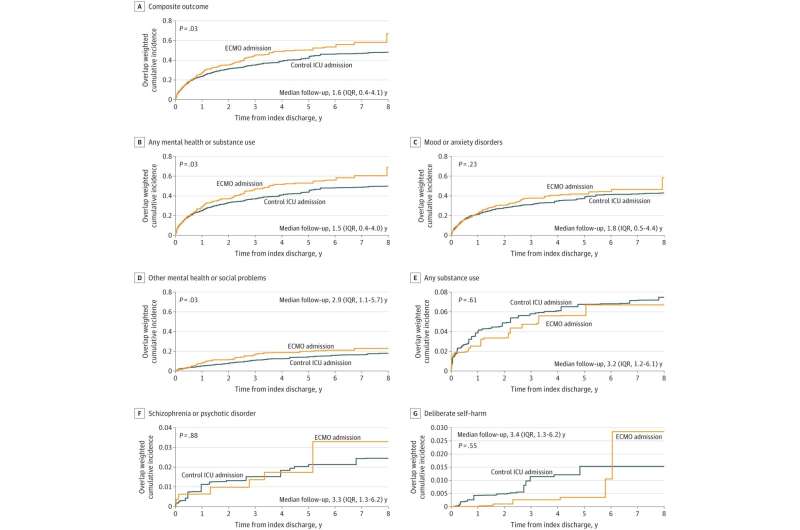
The researchers matched the 642 ECMO survivors with 3,820 other ICU survivors who had similar characteristics including age, sex, mental health history, critical illness severity and hospital length of stay. This analysis found ECMO patients had a 24% higher rate of new mental health diagnoses compared with other ICU survivors.
Of the 642 ECMO survivors, 236 (37%) were diagnosed with a new mental health condition. The most frequent diagnoses were depression, anxiety, and mental health conditions caused by a traumatic experience, known as traumatic disorders. Previous studies have found these to be the most common mental health diagnoses among survivors of critical illness.
“As care providers, we can tell our patients that it’s common to struggle with your mental health after an ICU admission,” said Dr. Peter Tanuseputro, co-senior author, physician-scientist at The Ottawa Hospital and ICES, investigator at the Bruyère Research Institute and associate professor at the Department of Medicine, University of Ottawa. “ICU survivors need to realize that they often face months or years of recovery, and families and healthcare providers need to support them.”
This study’s findings are particularly relevant during the COVID-19 pandemic, as the use of ECMO grew worldwide to address never-before-seen numbers of patients with severe respiratory failure. At the height of the pandemic, the province of Ontario had twice as many patients on ECMO as it did pre-pandemic.
“We suddenly have a lot more ECMO survivors because of COVID-19. We need to make sure they have the mental health support they need to recover and thrive,” said Dr. Kwadwo Kyeremanteng, co-senior author on the paper and scientist and critical care physician at The Ottawa Hospital, senior clinician investigator at the Institut du Savoir Montfort and assistant professor at the University of Ottawa.
The exact reasons why ECMO survivors are at greater risk of mental health problems compared to other ICU survivors is still unclear, and more research is needed.
Source: Read Full Article


