Researchers from the Netherlands conducted an observational study to determine the association between personal continuity and potentially inappropriate prescriptions (PIPs) by family physicians in older patients. PIPs can be categorized as potentially inappropriate medications (PIMs) and potential prescribing omissions (PPOs).
The study utilized anonymized routine care data from 269,478 patients, receiving care in 48 Dutch family practices, from 2013 to 2018. They included all patients 65 and older with five or more contacts with their practice in six years, giving them a sample of 25,854 individuals. Personal continuity was measured using three established indices: Usual Provider Continuity (UPC); the Bice-Boxerman Continuity of Care Index (BBI); and the Herfindahl Index (HI).
The prevalence of PIPs were determined using screening tools. To assess the association, they conducted analyses with and without adjustment for number of chronic conditions, age and sex.
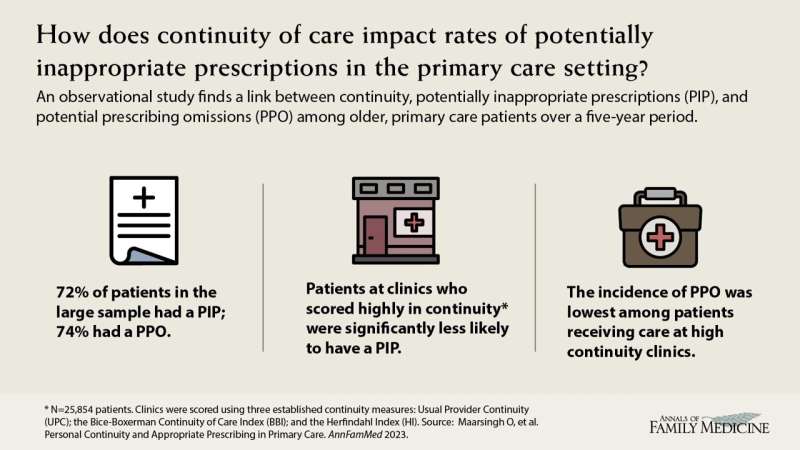
Higher scores in BBI, HI and UPC were associated with a significant reduction in potentially inappropriate prescriptions. Within the UPC, BBI and HI measures, the mean personal continuity was 0.70 (0.19), 0.55 (0.24) and 0.59 (0.22), respectively. Among more than 25,000 patients the researchers examined, 72.2% and 74.3% had one or more potentially inappropriate medications (PIMs) or PPOs, respectively; and 30.9% and 34.2% had three or more PIMs or PPOs, respectively.
The authors conclude that higher personal continuity is associated with more appropriate prescribing and argue that increasing personal continuity may improve quality of prescriptions and reduce harmful consequences.
Prescription management is an important aspect of primary care for older patients as inappropriate prescribing can result in avoidable adverse events such as hospitalizations, falls and acute kidney injury.
Researchers found a significant association between increased rates of primary care continuity, as measured by three indices, and a decrease in potentially inappropriate prescriptions (PIPs) among primary care patients. For potentially inappropriate medications (PIMs), this effect was only observed in the patient group with five to 18 chronic conditions compared to the groups with fewer chronic conditions.
The study is published in The Annals of Family Medicine journal.
More information:
Marije T. te Winkel et al, Personal Continuity and Appropriate Prescribing in Primary Care, The Annals of Family Medicine (2023). DOI: 10.1370/afm.2994
Journal information:
Annals of Family Medicine
Source: Read Full Article


