
More than 20,000 new coronavirus cases have emerged each day on average in Massachusetts for the past week. But in the bowels of Boston, there is a hint that the omicron-fueled surge may be on the verge of decline.
That glimmer of hope comes from an unlikely place: wastewater.
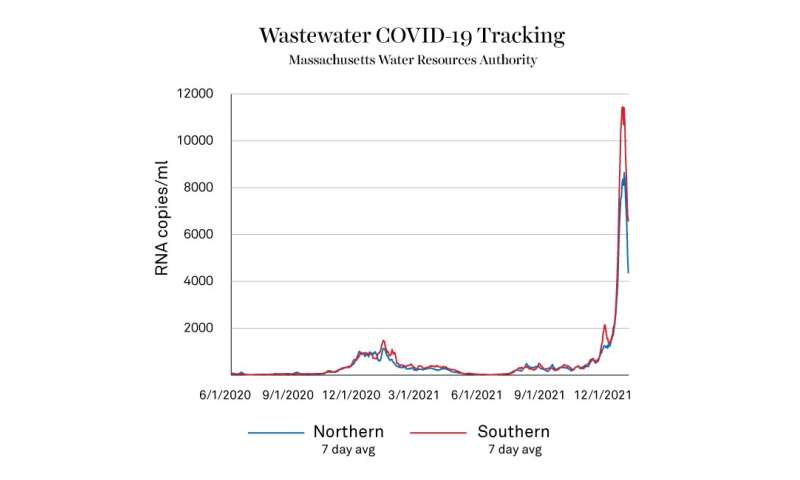
The coronavirus levels detected in samples from the Deer Island water treatment plant, which processes wastewater from communities around Boston and eastern Massachusetts, show a steep drop in recent days.
What can coronavirus levels in wastewater tell us about the omicron wave?
“Looking at wastewater readings is an important piece of the puzzle,” says Neil Maniar, director of the master of public health program, associate chair of the department of health sciences, and professor of public health practice at Northeastern. But “the interpretation of the wastewater data is much more complex than when folks look at the regular case counts.”
Case counts are fairly straightforward. Someone took a test that returned a binary result: Either the test detected SARS-CoV-2, the coronavirus that causes COVID-19, or it didn’t. Case counts gives a head count of the number of individuals in a population that reported a positive test result.
But there are all kinds of reasons that someone might not get tested or report their positive result to public health officials, says Maniar. They might be asymptomatic and not realize that they have been infected. Or maybe testing was inaccessible to them, or they couldn’t find the often-out-of-stock at-home antigen tests. Someone who takes a test at home also might not report a positive to authorities and simply quarantine on their own, too.
Wastewater readings offer something that case counts don’t.”Basically,” says Maniar, “everybody poops.”
“In a way, it’s the most comprehensive reading that we have,” he says. “It’s capturing everyone who is positive, as opposed to the testing data that are only capturing those who are tested and report it.”
But samples taken from city wastewater that has come from thousands of buildings can’t offer detailed information about who or how many people are infected. That’s because what scientists are actually measuring in a municipality’s wastewater is the concentration of bits of the virus.
The detection is similar to a nasal PCR coronavirus test, explains Jared Auclair, who runs Northeastern’s COVID-19 testing facility, the Life Sciences Testing Center in Burlington, Mass. When you swab inside your nostrils, you’re scraping off cells. If you’ve been infected, scientists can detect the presence of the virus’s RNA in those cells. Researchers also are looking for RNA from SARS-CoV-2 in wastewater. But in that case, no scraping is necessary.
“Your body’s job is to clear all foreign agents,” says Auclair, who is also associate dean of professional program and graduate affairs in the College of Science and an associate teaching professor of biotechnology at Northeastern. “That’s what’s happening. Your immune system is fighting off the virus and it’s got to go someplace. It can’t just hang out in your body. Generally speaking, we get rid of the stuff that we don’t need in our body through waste.”
By the time it reaches the wastewater, says Auclair, the virus is dead.
A big wrinkle in interpreting wastewater data is that everyone sheds virus differently, he says. Some people shed a lot of virus into wastewater, while others shed much less. And, he adds, there’s still a lot to learn about how people shed SARS-CoV-2. So the concentration of RNA from that coronavirus in wastewater is best treated as an average of what is going on in the population, rather than as a tool for individual decision-making.
Depending on how localized the data is, however, it could be an “indicator of the level of risk that exists in your community,” Maniar says. Or, he adds, it might add to demographic information about who is getting infected or at higher risk. But for now, most wastewater coronavirus tracking is happening at the large-scale level in cities.
The role for wastewater data in monitoring COVID-19, Maniar says, is largely as an early indicator of the trajectory of the pandemic. “It’s that early warning, that beacon that says, “Hey, we’ve got to do something about this, because there’s clearly something going on.'”
Part of the reason wastewater works well as an early warning system is because of the delay involved in testing. If you’re getting a PCR test, it can take days to get a result. If you’re taking a rapid antigen test, positive results generally show up later in the course of the infection. Or you might not think to get a test if you’re asymptomatic.
“You’re probably shedding virus before you have any symptoms,” Auclair says. “And we can see that in the wastewater.”
There was an exponential increase of SARS-CoV-2 in the Massachusetts wastewater from mid-March to mid-April 2020, followed by a decline, according to Biobot Analytics, the company conducting the tests. Four to ten days later, the number of cases and hospitalizations reported in Massachusetts rose dramatically. That was before testing was prevalent among asymptomatic people, so the timeline has likely shortened.
The more recent data from the Massachusetts Water Resources Authority coming out of the Deer Island Treatment Plant show that the concentration of the virus’s RNA has been falling over the past week. Readings of samples from the southern half of the system showed a seven-day average of 6,576 RNA copies/mL as of Tuesday, down from 11,446 RNA copies/mL on January 3. In the northern region, that metric fell to 4,365 RNA copies/mL on Tuesday down from a high of 8,644 RNA copies/mL on January 5.
“That’s a pretty significant decline in those numbers,” Maniar says. “That is a good sign that we’re moving in the right direction. But it’s going to be a little bit of time before we see those numbers reflected in case counts and in hospitalizations and other metrics.”
The sharp spike in COVID-19 cases is expected to be followed by an equally sharp decline, according to projections by Northeastern’s infectious-disease-modeling team. But hospitalizations are still high, and tend to lag a few weeks behind a change in case counts.
Source: Read Full Article


