The case for the use of intravenous iron therapy for some patients with heart failure (HF) and reduced ejection fraction (HFrEF) has strengthened in recent years, with several trials showing gains in surrogate outcomes such as exercise capacity and quality of life and one showing a 21% drop in risk for HF readmission or cardiovascular death.
Now, a small randomized trial may highlight a potential mechanism for those benefits by demonstrating what appears to be a direct salutary effect of the injectable iron preparation ferric carboxymaltose (Ferinject / Injectafer), or FCM, on reverse remodeling in iron-deficient patients with HFrEF.
In a novel research twist, the IRON-CRT trial included only patients with cardiac resynchronization therapy (CRT) implants, so it could leverage the devices for assessment of cardiac performance after 3 months of FCM therapy, its researchers say.
As a result, the trial “offers some mechanistic insights into the potential beneficial mode of action of ferric carboxymaltose in HFrEF patients,” said Pieter Martens, MD, of Oost-Limburg Hospital, Genk, Belgium, when presenting the results at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting, conducted virtually and live in Florence, Italy.
Its patients, who were already receiving “very robust background medical therapy and robust device therapy consisting of CRT,” Martens observed, benefited with significant new cardiac reverse remodeling after 3 months of FCM treatment, compared to similar patients assigned to a standard-care control group. Their left-ventricular ejection fractions (LVEFs) went up and left-ventricular end-systolic volumes (LVESVs) went down. They also showed relative gains in exercise capacity and higher scores on the Kansas City Cardiomyopathy Questionnaire (KCCQ), which measures functional status.
The findings fit well with current understanding of iron deficiency and its effects on myocardial energetics, Martens explained. Iron deficiency can impair the reverse-remodeling benefit of CRT and blunt the heart’s positive force-frequency relationship (FFR) ― a measure of contractile mechanics that normally climbs exponentially with accelerating heart rate. Put another way, cardiac output at exercise testing tends to go up less in HFrEF patients with iron deficiency compared to those who aren’t iron deficient.
The IRON-CRT trial suggests that FCM iron repletion in such patients “improves cardiac performance and is capable of transforming the negative FFR into a positive FFR,” thereby boosting cardiac output and exercise capacity, said Martens, who is also lead author on the study’s June 29 publication in the European Heart Journal.
Because the trial was randomized and so can indicate causality, the report states, IRON-CRT suggests that “FCM offers incremental reverse remodeling.” Although it included only patients with progressive HFrEF despite intensive medical and device therapy, “there is no reason to believe that FCM would not have similar effects in other iron-deficient HFrEF patients.”
IRON-CRT may help explain the benefits of FCM therapy seen in HFrEF for mostly functional endpoints in such studies as CONFIRM-HF, FAIR-HF, and EFFECT-HF and for clinical outcomes in AFFIRM-AHF, agreed Frank Ruschitzka, MD, University Heart Center Zurich, in Zurich, Switzerland, for theheart.org | Medscape Cardiology.
Iron repletion with FCM can make “an impact that’s hard to deny. The question is, why? And I think this study may provide some insight. The volumes get better, the ejection fraction gets better, and we see some impact on reverse remodeling,” said Ruschitzka, who wasn’t part of IRON-CRT.
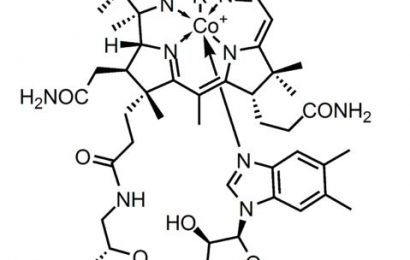
“It’s quite tempting to speculate that CRT and IV iron may work in synergy here,” which is certainly biologically plausible, he said when interviewed. “CRT is well established to upregulate mitochondrial proteins in the electron-transport chain,” a step in ATP creation that is fundamental to cardiac energetics, “and iron is an essential cofactor in that.”
IRON-CRT randomly assigned 75 iron-deficient patients whose LVEF was <45% while receiving CRT and who were stable in NYHA class II or higher on guideline-directed medical therapy to standard-care management either with or without FCM injections.
The study included only patients among whom the prevalence of biventricular pacing from CRT was at least 98% and for whom there was “almost universal use” of renin-angiotensin-system inhibitors, beta blockers, and mineralocorticoid receptor antagonists, Martens said.
The iron supplement was given over 12 weeks at standard doses that varied according to patient weight and hemaglobin level.
The least square mean change in LVEF at 12 weeks, the primary endpoint, was +4.22% absolute points for patients assigned to FCM but -0.23% in the standard-care group.
“This was driven by a significant reduction in left ventricular end-systolic volume [LVESV] in patients treated with ferric carboxymaltose, while the end-diastolic volume [LVEDV] remained virtually unchanged,” Martens noted.
Table. Changes* in Left Ventricular Systolic and Diastolic Volumes Over 12 Weeks, FCM vs No FCM
| Parameters | FCM, n = 37 | Standard Care Only, n = 38 | P value |
|---|---|---|---|
| LVESV (mL) | -9.72 | -1.83 | .001 |
| LVEDV (mL) | -2.5 | -1.9 | .748 |
| *Least-squares mean, in absolute mL units |
Cardiac performance in both groups at baseline was characterized by a negative FFR during biventricular pacing studies. The negative FFR became a positive FFR in the FCM group after 12 weeks of FCM therapy but remained negative in the standard-care group (P < .001).
Those who received FCM also showed significant improvements in peak VO2 (P = .023) and functional status as assessed on the KCCQ (P = .011). There were no significant differences in natriuretic peptide levels or prevalence of adverse events.
During a discussion following the Martens presentation at the ESC-HFA meeting, Petar Seferovic, MD, PhD, Belgrade University, Belgrade, Serbia, observed that peak VO2 improvements from FCM treatment in IRON-CRT were more pronounced than those seen in the EFFECT-HF trial, which did not include patients receiving CRT.
Patients in IRON-CRT may have been sicker than those in EFFECT-HF, Martens speculated, or perhaps it was because CRT protected them from chronotropic incompetence. With their CRT devices providing rate-adaptive pacing, “they were able to achieve very high heart rates,” so perhaps they “got a little bit more bang for their buck from ferric carboxymaltose.”
Martens has received fees for consulting and speaking, travel grants, and an unrestricted research grant from Vifor Pharma; disclosures for the other authors are in the report.
Eur Heart J. Published online June 29, 2021. Full text
Heart Failure Association of the European Society of Cardiology (ESC-HFA): Late-Breaking Trials 1. Presented June 29. 2021.
Follow Steve Stiles on Twitter: @SteveStiles2. For more from theheart.org | Medscape Cardiology, follow us on Twitter and Facebook.
Source: Read Full Article