Photo: Magnolia Regional Health Center
Cost is a major determining factor for patients deciding whether to pick up prescriptions from the pharmacy. When medications are too expensive, patients may abandon them, regardless of how important they are to their health.
THE PROBLEM
The impact of non-adherence is dire in terms of patient outcomes, with up to 125,000 avoidable deaths attributed to non-adherence every year, according to a New England Journal of Medicine study.
But what if prescribers and patients could view prescription drug costs and discuss options at the point of care to avoid “sticker shock” at the pharmacy counter? Would patients who are prescribed more affordable medications be more adherent than patients who are prescribed more expensive medications?
And could better adherence result in fewer avoidable emergency department visits and inpatient readmissions?
These are the questions Magnolia Regional Health Center in Corinth, Mississippi, asked as part of an initiative to improve outcomes for congestive heart failure patients, who are the highest source of the hospital’s readmissions.
“Physicians commonly prescribe antithrombotic or anticoagulants for these patients to prevent cardiac events such as heart attack and stroke, which may result in hospitalizations and readmissions if patients don’t adhere to their medication regimen,” said Brian Davis, CIO at Magnolia Regional Health Center.
PROPOSAL
Health IT vendor DrFirst’s applied clinical research team works with healthcare organizations to measure the impact of the company’s technologies, including improvements in clinical outcomes, clinical workflow and return on investment.
The DrFirst team worked with Magnolia Regional to create a study testing whether price transparency tools at the point of prescribing and prescription fill data could equip hospitalists and care navigator staff with vital information that would improve care for CHF patients.
“Having price transparency at the point of prescribing, and access to prescription fill data, can equip our hospitalists and care navigator staff with crucial information that could improve care for CHF patients.”
Brian Davis, Magnolia Regional Health Center
The vendor’s myBenefitCheck is a real-time price transparency tool that integrates with Magnolia Regional’s Meditech electronic health record. By connecting with the largest pharmacy benefits managers, the tool provides pricing information within the EHR’s prescribing workflow during the patient encounter.
“We wanted to test whether having this information would make patients more likely to adhere to their medication and care plans because they can afford the care prescribed for them,” Davis explained.
In addition, the vendor recommended MedHx, its medication history technology, to deliver the data providers would need for visibility into the prescription fill activity of patients in the study. MedHx would give clinicians access to 12 months of medication history data from multiple trusted sources and would rely on an AI engine to convert that data into the EHR without a lot of manual entry.
MEETING THE CHALLENGE
The hospitalists, care navigators and primary care providers worked together to roll out a three-step approach to better understand the impact of having drug costs available to physicians and patients at the point of care.
Step 1: Establish a baseline of clinical outcomes.
“Many studies have shown that lower medication adherence leads to much higher odds of CHF patients being readmitted to the hospital, and that interventions to improve medication adherence reduce readmission rates,” Davis noted. “With this in mind, the first step was to determine the baseline levels of medication adherence by patients who were readmitted versus those who were not readmitted.
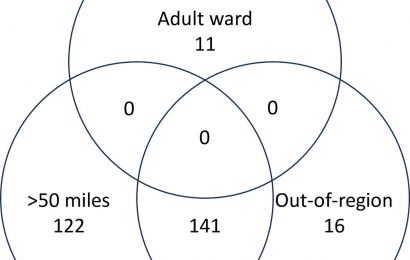
“All 417 patients in the study had been admitted to the hospital with a diagnosis of CHF,” he continued. “Of those patients, 84 (20%) were readmitted to inpatient care and 35 (8%) presented at the emergency department as a recurrent visit but were stabilized and sent home.”
Step 2: Determine which medications patients were not filling consistently.
“Next, it was important to determine the adherence levels of specific medications by patients who were readmitted versus those who were not readmitted,” Davis said. “Antithrombotic or anticoagulant medications are commonly prescribed to CHF patients following a hospitalization because they are very effective, but some can have incredibly high out-of-pocket costs to patients.”
To keep CHF patients out of the hospital, adherence to these medications is critical.
“The team theorized that if patients knew their out-of-pocket costs in the exam room, they could ask the provider to switch to a less expensive drug,” Davis said. “The lower cost might make them more likely to fill the prescription.”
Step 3: Implement new technologies.
“To test the impact of price transparency on how well patients adhere to their medication regimens, we collaborated with DrFirst’s applied clinical research team to gather and analyze medication history data,” Davis explained. “Then we installed myBenefitCheck into the real-time benefit check (RTBC) workflow in our EHR, which made more prescription benefit information and therapeutic alternatives available during the patient encounter.
“Next, we used MedHx to gather complete patient medication history so we could track whether patients in the study had filled their prescriptions,” he added.
RESULTS
From July 2020 to September 2021, Magnolia Regional studied medication adherence and prescription fill rates for 417 patients with CHF. When medications were broken down by drug class, first-fill prescription abandonment for more expensive antithrombotics was higher in readmitted patients (50%) than in non-readmitted patients (35%).
“Results found little difference in first-fill prescription abandonment for less expensive anticoagulants – 31% in readmitted patients versus 32% in non-readmitted patients,” Davis reported. “Readmitted patients were 10% less adherent to antithrombotic agents, however, and 17% less adherent to anticoagulants than patients who were not readmitted.
“By measuring prescription abandonment and adherence for these medications – which are vital to keeping patients out of the hospital – the team validated its assumption: Having price transparency at the point of prescribing and access to prescription fill data can equip our hospitalists and care navigator staff with crucial information that could improve care for CHF patients,” he continued.
Magnolia Regional is dedicated to empowering its providers with innovative technologies that support their ability to provide the highest quality of care to patients. The myBenefitCheck technology gives prescribers up-to-the-minute, patient-specific information on drug costs while they are face-to-face with patients, helping to minimize the financial obstacles that keep patients from filling their prescriptions, Davis said.
Then, using MedHx data, Magnolia Regional can track fill rates for these patients, pinpoint gaps in adherence and identify those at risk of readmission, he added.
ADVICE FOR OTHERS
“With prescription drug prices rising at every turn, patients need price transparency and the ability to discuss options with their doctors during office visits,” Davis advised. “To address this need, starting January 1, 2023, the Centers for Medicare & Medicaid Services will require insurers that offer Medicare Part D health benefits to use an electronic drug cost and health benefit comparison tool that’s compatible with at least one EHR system.
“The goal is to allow patients to compare the cost of prescription drugs, request a similarly effective option, and better understand what they will need to pay before they are standing at the pharmacy counter,” he continued.
“By reducing the frequency of prescription abandonment due to sticker shock, a real-time prescription benefit solution in tandem with complete medication history data can help hospitals and health systems address medication adherence challenges in vulnerable patient populations.”
Twitter: @SiwickiHealthIT
Email the writer: [email protected]
Healthcare IT News is a HIMSS Media publication.
Source: Read Full Article