As the coronavirus disease 2019 (COVID-19) pandemic continues, a number of different drugs have been examined for their potential efficacy in the prevention or alleviation of infection with the causative virus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A new Cellular and Molecular Life Sciences study discusses the possible role of melatonin, an antioxidant and anti-inflammatory agent, in treating COVID-19.
Study: Melatonin: Highlighting Its Use as A Potential Treatment For SARS-Cov-2 Infection. Image Credit: Vikks / Shutterstock.com
Introduction
Melatonin has been the focus of much research throughout the COVID-19 pandemic, as it is a safe molecule with many clinical actions that could be beneficial to humans. Moreover, melatonin is a biomolecule that is naturally produced in the human body and is associated with a broad spectrum of antiviral activity. Despite its demonstrated safety and efficacy in reducing COVID-19 severity, there has been little interest shown by pharmaceuticals or governments in extending its use.
This is in sharp contrast to more heavily publicized, expensive, and toxic/less safe treatment modalities, such as remdesivir, glucocorticosteroids, and azithromycin. Thus, the current study reviews the evidence for the use of melatonin in treating COVID-19.
Earlier studies have found that melatonin is useful in preventing bacterial sepsis, especially in premature newborns with septic shock or bacterial sepsis. Moreover, higher levels of melatonin in the body have been associated with resistance to brucellosis.
The pathogenesis of severe COVID-19
Severe and critical forms of COVID-19 are attributed to the hyperinflammatory response evoked by SARS-CoV-2, or as a result of the immune reaction to the virus or its components. Either way, this immune e response to SARS-CoV-2 initiates a massive and uncoordinated release of tissue-damaging cytokines and complement factors that are responsible for the clinical features of a progressive and often fatal disease.
In COVID-19, the toxic phospholipase sPLA2-IIA is very high, leading to detrimental changes in biomembranes by the hydrolysis of fatty acids. The release of arachidonic acid stimulates the cyclooxygenase pathways, causing the generation of inflammatory mediators like prostacyclins and prostaglandins. This drives the production of reactive oxygen species (ROS)/reactive nitrogen species (RNS), which are damaging to cell and nuclear membranes, as well as DNA.
Injury to the mitochondrial membranes leads to energy deficits. Secondary infection of SARS-CoV-2-infected lungs with bacteria/fungi could lead to synergistic injury by enhancing cytokine release, resulting in acute respiratory distress syndrome. In this situation, melatonin appears to be a useful agent.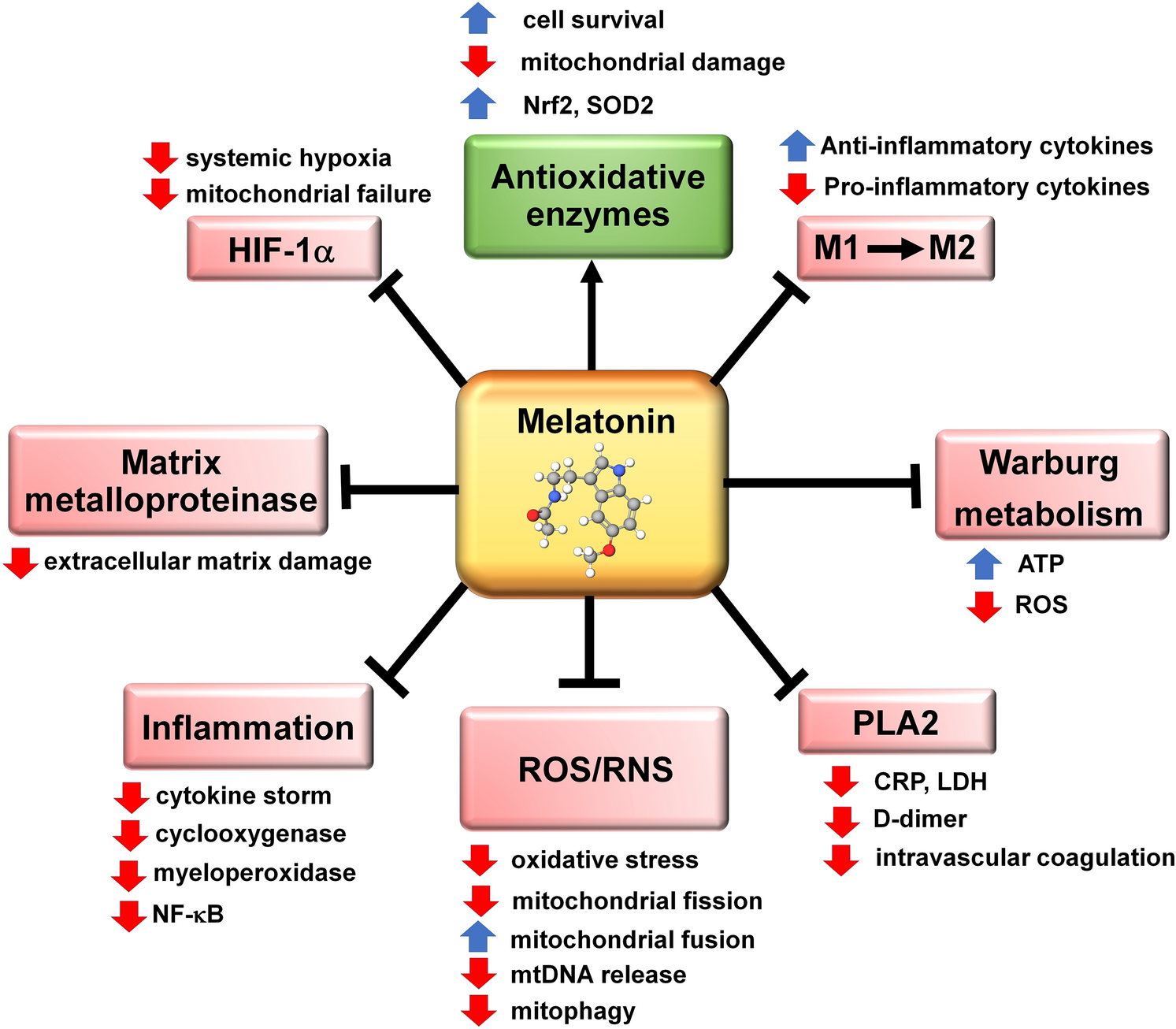
The actions of melatonin that contribute to the ability of this ubiquitously distributed molecule in reducing the severity of a SARS-CoV-2 infection. HIF-1α = hypoxia-inducible factor 1 alpha; M1 = pro-inflammatory macrophage; M2 = anti-inflammatory macrophage; mtDNA = mitochondrial DNA; NF-ҝB = nuclear factor kappa B; Nrf2 = transcription factor NF-E2 p45 transcription factor; PLA2 = phospholipase A2; RNS = reactive nitrogen species; ROS = reactive oxygen species; SOD2 = superoxide dismutase 2. Pointed arrow = stimulation; blunt arrows = inhibition
An overview of melatonin
Melatonin is a molecule with high anti-inflammatory and antioxidant activity. This molecule blocks a variety of pathways triggered by cell damage or inflammation.
More specifically, melatonin blocks ROS/RNS pathways, thus mitigating oxidative stress and damage to the cells, preventing mitochondrial fission and encouraging mitochondrial fusion, blocking the release of mitochondrial DNA, and preventing mitophagy, which is the phagocytosis of mitochondria.
Melatonin thus enhances the synthesis of adenosine triphosphate (ATP), while reducing ROS levels. By inhibiting the enzyme matrix metalloproteinase (MMP) in the extracellular space, melatonin prevents damage to the matrix supporting cells within the tissue.
During septicemia, activated immune cells shift their metabolic profile from oxidative phosphorylation within the mitochondria to glycolysis within the cytoplasm through a process known as Warburg metabolism. Herein, macrophages shift from the M2 anti-inflammatory phenotype to M1 pro-inflammatory cells, thereby contributing to the hyper-inflammatory profile.
The key factor may be the changes in mitochondrial structure and function, which reduces cellular and organismal death.
How melatonin can treat COVID-19
With severe COVID-19, hypoxic damage is mediated by hypoxia-inducible factor (HIF)-1α, a marker of increased mortality. In fact, the rise HIF-1α in diabetics is a key contributor to the severity of COVID-19 in this subset of patients, as high glucose levels stimulate glycolysis within the inflammatory macrophage-monocyte cell subset.
This enhances viral replication, causing high ROS levels while stabilizing high HIF1-α levels. Subsequently, glycolysis levels rise, which also causes cytokine levels to increase in a dysregulated manner.
The activity of HIF-1α is suppressed by melatonin, which reverses the Warburg metabolic shift while also inhibiting the inflammasome and macrophage changes. This prevents the cytokine storm, inhibits pro-inflammatory enzymes cyclo-oxygenase and myeloperoxidase, and suppresses the inflammatory signaling molecule nuclear factor κB (NF-κB). This leads to increased cell survival, lower levels of lung damage, less mitochondrial damage, and higher levels of transcription factors and of superoxide dismutase 2 (SOD2).
Some researchers think that the elderly are more prone to severe COVID-19 because of their lower melatonin production levels. With Warburg metabolism, intracellular glucose enters the cytosol for glycolysis, rather than remaining in the mitochondria for oxidative phosphorylation. The resulting deficit of acetyl coenzyme A (CoA), a product of this cycle, leads to the inhibition of melatonin synthesis within the mitochondria.
Implications
Clinically, melatonin treatment reduces the severity of SARS-CoV-2 infections in terms of lowering the seriousness of symptoms, decreasing the need for hospitalization (which simultaneously helps control health care exhaustion), reducing the duration of hospital stay when this is necessary, eliminating the need for mechanical intubation, and lessening the death rate.”
To date, several clinical trials are currently being conducted to assess the efficacy of melatonin at doses from 2 mg to 500 mg daily, given to patients with varying levels of severe COVID-19. Earlier studies failed to show any toxicity, even at the highest doses used. Moreover, melatonin was predicted to be most likely to control SARS-CoV-2 infection.
Future trials should include children and other people over a wide age spectrum to improve the generalizability of these results. Once the key facts of melatonin treatment are resolved, supplementation of melatonin could help protect cells and mitochondria against inflammatory damage through the Warburg effect.
The authors of the current study indicate that melatonin has at least twice the efficacy of remdesivir or tocilizumab in reducing inflammatory markers in COVID-19. Both remdesivir and tocilizumab are currently being used under certain clinical constraints to treat COVID-19, though both have significant adverse reactions and must be given intravenously. Conversely, melatonin can be given orally and by any other route, without causing any known toxicity.
In the current scenario where vaccine resistance is rising and vaccine distribution to remote areas of the world is limited, melatonin, used alone or along with vaccines/antivirals, could be part of the answer.
The use of melatonin would be especially advantageous because it can be orally self-administered, it is low in cost, and it lacks significant toxicity. This applies especially to impoverished regions of the world where the populace has fewer financial resources to devote to the treatment of this disease and where health care is not readily available.“
- Reiter, R. J., Sharma, R., Simko, F., et al. (2022). Melatonin: Highlighting Its Use as A Potential Treatment For SARS-Cov-2 Infection. Cellular and Molecular Life Sciences. doi:10.1007/s00018-021-04102-3.
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Acute Respiratory Distress Syndrome, Adenosine, Adenosine Triphosphate, Anti-Inflammatory, Antioxidant, Arachidonic Acid, Azithromycin, Bacteria, Brucellosis, Cell, Children, Coronavirus, Coronavirus Disease COVID-19, Cytokine, Cytokines, Cytoplasm, DNA, Drugs, Efficacy, Enzyme, Exhaustion, Fatty Acids, fungi, Glucose, Glycolysis, Health Care, Hospital, Hypoxia, Inflammasome, Inflammation, Intracellular, Lungs, Macrophage, Melatonin, Metabolism, Mitochondria, Molecule, Monocyte, Mortality, Myeloperoxidase, Oxidative Stress, Oxygen, Pandemic, Phagocytosis, Pharmaceuticals, Phenotype, Phosphorylation, Remdesivir, Research, Respiratory, SARS, SARS-CoV-2, Sepsis, Septic Shock, Septicemia, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stress, Syndrome, Transcription, Transcription Factors, Vaccine, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article


