Led by the London School of Hygiene & Tropical Medicine (LSHTM), in partnership with the World Health Organization (WHO) and Avenir Health, the research team carried out a systematic review and meta-analysis of syphilis prevalence among MSM between 2000 to 2020, drawing on data from 275 studies involving more than 600,000 study participants across 77 countries.
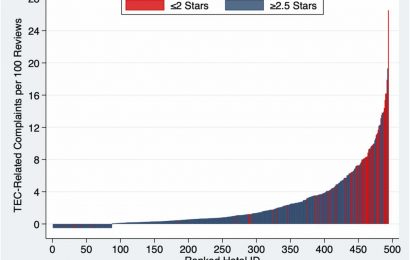
The worldwide prevalence of syphilis among MSM was 15x higher than most recent estimates for men in the general population (7.5% versus 0.5%). Researchers further estimated the prevalence across eight regions of the Sustainable Development Goals (SDG) and six regions of the WHO. Latin America and the Caribbean region had the highest prevalence of syphilis (10.6%), whereas Australia and New Zealand had the lowest (1.9%). There is, therefore, an urgent need to quantify the burden of syphilis in this high-risk group.
Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum. When diagnosed, syphilis is easily treated with penicillin. One study found that annual screening and treatment of at least 62% of sexually active MSM is necessary to achieve local elimination.
Dr. Matthew Chico, Associate Professor at LSHTM and lead author, said: “Men tend to be disadvantaged when it comes to syphilis testing and treatment. Women are routinely screened for syphilis at their first antenatal care visit, and are offered testing at family planning services. Men in general do not have the same number of contacts with the health system as women, and MSM face additional barriers due to stigma and shaming.
“As diseases go, syphilis is terribly deceptive. In the primary and secondary stages of infection, skin lesions, such as chancre or rash, may present, only to then disappear as if the person has been cured. Unfortunately, without treatment, the bacterium will slowly invade internal organs, and can lead to physical deformity, loss of vision, dementia, and even death. There is no good reason for this to happen. We have effective treatment.”
Dr. Motoyuki Tsuboi, from LSHTM and the study’s first author, said: “The Global Health Sector Strategy of the WHO has an ambitious target to reduce global syphilis incidence by 90% between 2018 and 2030. We hope our findings—the first global prevalence estimates of syphilis among MSM—will serve as a catalyst for action.”
In this new study, pooled estimates of syphilis among MSM were highest (8.7%) in regions where HIV prevalence is more than 5%. Lower-middle income countries also had a high burden (8·7%). Countries with low-income status had the lowest syphilis prevalence estimates among MSM (3.8%). Syphilis prevalence estimates were high among studies exclusively involving male sex workers, transgender women, and transgender women sex workers.
Among studies conducted from 2000 to 2009 and 2010 to 2020, global syphilis prevalence was estimated to be 8·9% and 6·6% respectively. However, four of eight SDG regions—Europe and Northern America, Latin America and the Caribbean, Oceania [excluding Australia and New Zealand]) – showed higher estimates between 2015 and 2020 than 2010 and 2014.
Dr. Tsuboi said: “Syphilis prevalence among MSM is unacceptably high at the global and SDG regional levels, particularly in lower-middle, upper-middle, and high-income countries, where cases appear to be increasing and where HIV prevalence is high. Urgent action is needed.”
The researchers say that it is difficult to know if syphilis prevalence among MSM will be altered by the COVID-19 pandemic. While there is evidence the pandemic has impacted MSM sexual activity, there have also been reports that MSM have experienced difficulty accessing STI testing and treatment due to COVID-19, potentially translating into fewer syphilis cases being diagnosed, treated and removed from the MSM population.
Eloise Stonborough, Associate Director of Policy and Research at Stonewall, (she/her) said: “Sexually transmitted infections, including syphilis, can cause severe health problems if untreated. These figures provide an important insight into the increased prevalence of syphilis infections for men who have sex with men. It’s important that everyone, including LGBTQ+ people and those at higher risk, is supported to understand how to protect themselves against syphilis and other sexually transmitted infections.
“It’s also vital that healthcare services are inclusive and welcoming of all lesbian, gay, bi, trans and queer people, so everyone feels comfortable getting the help and support they need.”
Source: Read Full Article