University of Minnesota researchers and their collaborators at the National Cancer Institute (NCI) investigated the role of a new intracellular checkpoint gene in regulating T-cell function against solid tumors. Known as CISH, the team published results in Med that show the checkpoint gene plays a key role in suppressing the ability of human T-cells to recognize and attack cancer cells.
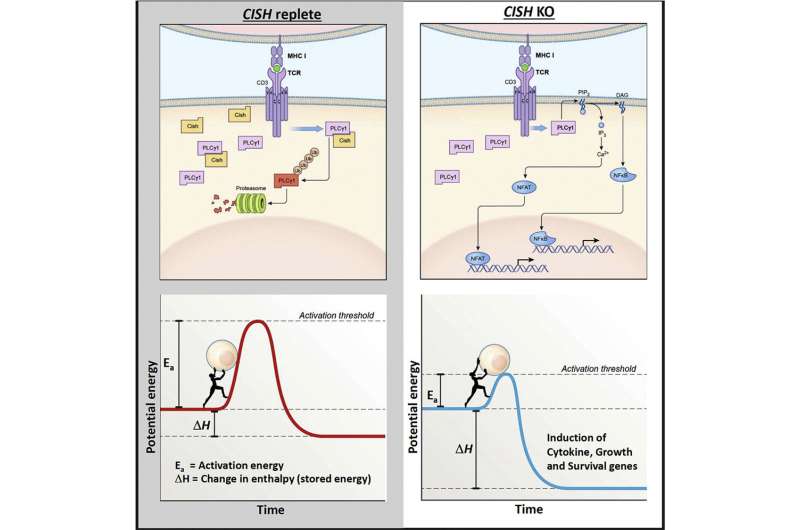
When CISH is disabled, T-cells more effectively recognize mutated proteins produced by tumors. CISH inhibition also preserved T-cell fitness and made T-cells more responsive to existing checkpoint therapies, suggesting a new avenue to make breakthroughs in cancer immunotherapy.
“It is a true bench-to-bedside story that is currently being deployed in patients with metastatic gastrointestinal cancer who have exhausted virtually all other treatment options,” said Beau Webber, Ph.D., an assistant professor at the University of Minnesota Medical School and member of the Masonic Cancer Center. “We are applying what we found in the lab to patients seeking care for gastrointestinal cancer.”
As CISH resides within the cell, it cannot be inhibited using antibody blockades in the same way that other checkpoint molecules have been targeted. To overcome this challenge, the research team led by University faculty Branden Moriarity, Ph.D., and Dr. Webber utilized CRISPR gene editing—a process of cutting a DNA sequence to delete and insert other sequences—to safely and effectively knockout the CISH gene in human T-cells. This process robustly enhanced T-cells’ ability to recognize and kill tumor cells, and served as the preclinical basis for the first-in-human clinical trial using CRISPR engineered T cells at the University of Minnesota—only the second CRISPR clinical trial authorized by the Food and Drug Administration at the time.
“This work is the culmination of a tremendous, multidisciplinary effort encompassing basic mechanistic immune biology, cutting-edge techniques in genome editing, and the latest advancements in adoptive cellular immunotherapy,” said Dr. Webber.
Gene editing offers a powerful new tool that allows researchers to hard-wire checkpoint inhibition into the specific immune cells that are fighting the tumor, thereby accelerating clinical translation of new approaches. Intracellular checkpoint genes, like CISH, are of particular interest because they offer a new avenue to enhance immune cell function against cancer.
Source: Read Full Article


