- Immune-mediated and autoimmune diseases are linked with the irregular activity of the immune system. Common examples of these diseases include psoriasis, rheumatoid arthritis, multiple sclerosis, and type 1 diabetes.
- A recent perspective piece in the journal Science suggests that obesity may contribute to autoimmune disease risk due to overactive nutrient and energy-sensing pathways.
- The author of the essay suggests that reducing caloric intake and using certain medications may help counteract the associated risk for autoimmune diseases from obesity.
The immune system’s role is to defend against what is dangerous to the body. However, it does not always work as it should, which can lead to health problems.
There is a great need for research to understand what triggers autoimmunity — where the body turns against itself or acts abnormally.
A recent perspective piece published in Science by Dr. Giuseppe Matarese, a professor of immunology at the University of Naples Federico II in Naples, Italy, discusses how obesity and overnutrition could influence the regulation of the immune system.
Autoimmune, immune-mediated diseases
Note: There is a difference between autoimmune conditions and immune-mediated conditions. The term “immune-mediated” is an umbrella term for disorders with abnormalities in immune system activity. Autoimmune diseases are a subcategory of immune-mediated diseases. Expert commenters and the perspective piece author have chosen to use the term “autoimmune disorders” as an umbrella term instead of “immune-mediated.”
Over 23.5 million people in the United States have some type of autoimmune disease. Autoimmune diseases occur when the body’s immune system attacks healthy body tissues.
The specific tissues affected will impact how the disease develops and doctors’ treatment approaches. For example, psoriasis is an autoimmune disease that affects the skin, while hemolytic anemia damages the body’s red blood cells. Inflammation is a common component of many autoimmune diseases.
It is not completely clear what causes autoimmune and immune-mediated diseases. Research is ongoing to understand modifiable and non-modifiable risk factors.
For example, someone’s genetics may play a role in developing an autoimmune disease, but so can certain lifestyle choices. One area of interest is how diet and weight may affect the risk for autoimmune and immune-mediated diseases.
Dr. Jason Balette, a bariatric surgeon with Memorial Hermann in Houston, TX, explained to Medical News Today:
“There appears to be a clear correlation with obesity and autoimmune diseases like MS. This association has been demonstrated through cell signal pathways between adipose cells (fat cells) and the immune system. Just as malnutrition has been shown to decrease immune function, overnutrition (obesity) has been demonstrated to increase immune function leading to autoimmune diseases. Clearly, there is much to learn about these relationships and cell signals to help guide us with treatment plans in the future.”
Obesity as a factor in autoimmune disease
The perspective paper in Science looked at how excessive caloric intake and obesity may influence the risk for abnormal immune responses by the body.
Dr. Matarese wrote about the possible underlying mechanisms of obesity and excessive caloric intake that may affect the body’s immune response.
He proposed that people who consume an obesogenic Western diet, that is, a diet that can lead to obesity, have changes in their metabolic workload. Put simply, they experience metabolic overload, which has many implications at the cellular level.
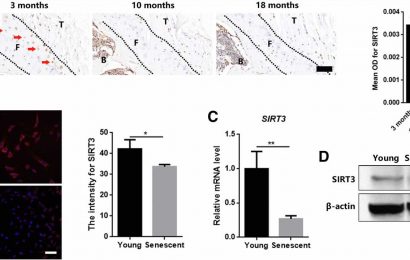
First, he proposed that adipose tissues promote increased leptin and cytokine levels. Leptin is a hormone that influences hunger and appetite. Cytokines influence the activity and production of immune cells.
He further notes that the circulation of certain nutrients from high-calorie intake in obese individuals is also at work.
He proposed that these three factors combined lead to increased inflammatory response and abnormalities in the actions and cells of the immune system. These results then lead to an increased risk for autoimmune disorders.
Dr. Matarese explained some of the critical points of his paper to MNT:
“This perspective summarizes why today we observe a raising in frequency of autoimmune diseases in more affluent countries where there is a strong excess of calorie intake. Calories in excess induce activation of immune cells, thus leading to an increased chance to loose immunological self-tolerance. Generally, the amount of calories and the quality of foods, typically of western diets rich in lipids and carbs, induce inflammation by activating innate and adaptive immune cells and their production of inflammatory mediators, increasing the chance of developing autoinflammation.”
Continuing research and interventions
Based on the ideas he presents in the piece, Dr. Matarese suggests that behavioral interventions may help control the body’s autoimmune response. This could involve intermittent fasting and calorie restriction. It could also include using medications that mimic fasting and reduce the body’s inflammatory response.
Dr. Matarese also discussed that researchers need to go further in investigating different areas. “[We need to] understand specifically if specific diet regimens, not only the amount of calories, predispose to specific diseases more than others,” he told MNT.
Researchers should “also assess whether calorie restriction (CR) can be an effective additional treatment to improve autoimmunity together with specific drug treatments — i.e. there are ongoing trials associating calorie restriction to treat multiple sclerosis together with drugs such as dimethyl fumarate,” he added.
Commenting on the paper, Dr. Balette noted that it points to the importance of maintaining a healthy body weight and what further research could include. He elaborated to MNT:
“The connection between obesity and autoimmune diseases as well as other medical comorbidities related to obesity demonstrates the importance of the need for both surgical and non-surgical weight loss. The further research areas I would like to see would be the continued investigation of the cell signals like leptin, ghrelin and how they change in the post-operative bariatric surgical patient. In addition, further investigation with immunosuppressive and anti-inflammatory drugs and how they function in the obese patient.”
Source: Read Full Article