In a recent study posted to the bioRxiv* preprint server, researchers in Australia explored the molecular mechanisms of the pulmonary and cardiac complications caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection using human stem-cell-derived cardiac and lung cells.
 Study: Parallel use of pluripotent human stem cell lung and heart models provide new insights for treatment of SARS-CoV-2. Image Credit: Kateryna Kon / Shutterstock
Study: Parallel use of pluripotent human stem cell lung and heart models provide new insights for treatment of SARS-CoV-2. Image Credit: Kateryna Kon / Shutterstock
Background
Although the coronavirus disease 2019 (COVID-19) has primarily affected the respiratory and pulmonary systems, severe COVID-19 manifestations have also affected the cardiovascular, digestive, renal, and nervous systems.
Magnetic resonance imaging (MRI) and electrocardiographs (ECG) have detected cardiac complications such as myocardial injury, arrhythmias, and thromboembolisms in a large number of recovering COVID-19 patients. In addition, autopsies have also detected spike (S) protein antigen and SARS-CoV-2 RNA in the heart tissue of patients who succumbed to COVID-19.
The SARS-CoV-2 S protein initiates infection by binding to the angiotensin-converting enzyme 2 (ACE2) receptor on the host cell surface. Host cell proteases such as furin cleave the S protein into two subunits — S1 and S2. The subsequent fusion of the viral and host cell membranes requires the cleavage of S1 from S2 by serine proteases or cathepsins. Tissue tropism of the virus is determined by the expression of either ACE2 and serine proteases, or ACE2 and cathepsins, which differs across the respiratory, pulmonary, cardiac, renal, and digestive systems.
About the study
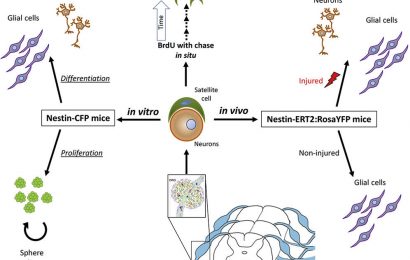
The present study used human pluripotent stem cells (hPSCs) to generate functional lung and heart cells. The stem cell-derived cardiac cultures and lung alveolar type II (AT2) epithelial cells could be infected with SARS-CoV-2. Vero cells or African green monkey kidney epithelial cells, extensively used in COVID-19 research, were also used in this study for comparisons.
These cells were used in paired experiments to determine the similarities and differences in mechanisms and factors influencing COVID-19 manifestations in the lungs and the heart.
The team used clustered regularly interspaced short palindromic repeats (CRISPR)-associated protein 9 (Cas9) mediated knockout of the ACE2 receptor to understand its importance in SARS-CoV-2 infection. Additionally, small molecule inhibitors were used to tease out the different mechanisms of viral entry. They also used phosphoproteomics and transcriptome profiling to understand differences in cellular responses during SARS-CoV-2 infections.
Results
The study's significant findings indicated that while all three cell types were dependent on the presence of ACE2 receptors, the downstream processing of the viral S protein was along different pathways. For example, in lung AT2 cells, the cleavage of the S protein was carried out by TMPRSS2 serine proteases on the host cell membrane, while the viral entry into heart cells was through the endosomal pathway through cathepsin-mediated cleavage of the S1 and S2 subunits.
Entry inhibition assays using TMPRSS2 inhibitor Camostat mesylate prevented SARS-CoV-2 infection of lung AT2 cells, highlighting the role of serine proteases in the viral entry in lung cells. Similar assays with CA-074 Me, a Cathepsin B and L inhibitor, blocked viral entry into cardiac cells.
Aborted SARS-CoV-2 infection in knockout ACE2 lung and heart cells demonstrated that ACE2 receptors were essential for viral infection. However, using a combination of anti-ACE2 antibodies blocked SARS-CoV-2 infection in lung and heart tissue, but low doses of anti-ACE2 antibodies prevented viral infection only in cardiac cells. These results, combined with ribonucleic acid (RNA) sequencing and quantitative polymerase chain reaction (qPCR) analyses, showed that lung AT2 cells had a higher expression of ACE2 receptors than cardiac cells.
Furthermore, the viral infection resulted in a strong interferon response in cardiac cells but not lung AT2 cells. The results from the phosphoproteomics analysis also showed that the infection activated different pathways in lung AT2 and cardiac cells.
Conclusions
Overall, the results revealed significant differences in the mechanism of SARS-CoV-2 infection in cardiac and pulmonary cells and tissue. While viral entry begins in both cells with ACE2 receptor binding, subsequent pathways of viral infection differ considerably with the spike protein undergoing serine protease cleavage in lung AT2 cells and endosomal cathepsin cleavage in cardiac cells.
The authors believe that the differential spike protein cleavage and the variance in ACE2 receptor expression in both these cells indicate the need for improved antiviral therapy and the inclusion of combinations of drugs to target both endosomal and membrane protease pathways of viral entry. They suggest using drugs that target serine/arginine-rich splicing factor protein kinase-1 (SRPK1) and cyclin-dependent kinases (CDK).
The study also highlighted the importance of using stem-cell-derived cell models other than immortalized cell lines like Vero cells to test the antiviral efficacy and cytotoxicity of COVID-19 therapies.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Parallel use of pluripotent human stem cell lung and heart models provide new insights for treatment of SARS-CoV-2: Rajeev Rudraraju, Matthew J Gartner, Jessica A Neil, Elizabeth S Stout, Joseph Chen, Elise J Needham, Michael See, Charley Mackenzie-Kludas, Leo Yi Yang, Mingyang Wang, Hayley Pointer, Kathy Karavendzas, Dad Abu-Bonsrah, Damien Drew, Yu Bo Yang Sun, Jia Ping Tan, Guizhi Sun, Abbas Salavaty, Natalie Charitakis, Hieu T Nim, Peter D Currie, Wai-Hong Tham, Enzo Porrello, Jose Polo, Sean J Humphrey, Mirana Ramialison, David A Elliott, and Kanta Subbarao. bioRxiv. 2022. DOI: https://doi.org/10.1101/2022.09.20.508614, https://www.biorxiv.org/content/10.1101/2022.09.20.508614v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antigen, Arginine, Cas9, Cell, Cell Membrane, Coronavirus, Coronavirus Disease COVID-19, covid-19, CRISPR, Cytotoxicity, Drugs, Efficacy, Enzyme, Heart, Imaging, Interferon, Kidney, Kinase, Knockout, Lungs, Magnetic Resonance Imaging, Membrane, Molecule, Palindromic Repeats, Polymerase, Polymerase Chain Reaction, Protein, Receptor, Research, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Serine, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Splicing, Stem Cells, Syndrome, Virus
.jpg)
Written by
Dr. Chinta Sidharthan
Chinta Sidharthan is a writer based in Bangalore, India. Her academic background is in evolutionary biology and genetics, and she has extensive experience in scientific research, teaching, science writing, and herpetology. Chinta holds a Ph.D. in evolutionary biology from the Indian Institute of Science and is passionate about science education, writing, animals, wildlife, and conservation. For her doctoral research, she explored the origins and diversification of blindsnakes in India, as a part of which she did extensive fieldwork in the jungles of southern India. She has received the Canadian Governor General’s bronze medal and Bangalore University gold medal for academic excellence and published her research in high-impact journals.
Source: Read Full Article