Mechanisms involved in the rapid, severe progression of fibrosis in the lung tissues of COVID-19 patients, a potentially fatal complication of the virus that damages and scars the lungs, have been uncovered by researchers led by UTHealth Houston.
Until now, little was known about the cellular mechanisms that lead to fulminant lung fibrosis (FLF) in non-resolvable COVID-19. FLF is characterized by the sudden onset and rapid progression of damage to lung tissue, often requiring lung transplantation.
“We believe this is the initial step to understanding post-ARDS fibrosis from COVID-19 and potentially offers us insight into potential therapies for this disease,” said Soma S.K. Jyothula, MD, senior author on the study, and associate professor in the Center for Advanced Cardiopulmonary Therapies and Transplantation at McGovern Medical School at UTHealth Houston.
Of those patients with COVID-19 pneumonia, severe lung disease and acute respiratory distress syndrome (ARDS) has been a primary cause of death since the pandemic began in 2020, Jyothula said.
Evidence of FLF can be seen on average about 15 weeks after symptom onset, according to the study published online by eBio Medicine.
Symptoms of FLF of post-COVID-19 ARDS include severely low levels of oxygen in the tissues requiring high amounts of oxygen supplementation, the need for mechanical ventilation, and occasionally support from a machine that oxygenates the patient’s blood outside of the body, then returns it to their system.
The research revealed a unique fibrotic gene signature in non-resolvable COVID-19 patients; they describe non-resolvable as patients who experienced prolonged pulmonary effects following infection with the virus.
“In some patients with COVID-19, lung injury can progress rapidly to the point that lung transplantation is the only viable option for survival,” said Jyothula, the Graham Distinguished Professor in Pulmonary Medicine at McGovern Medical School.
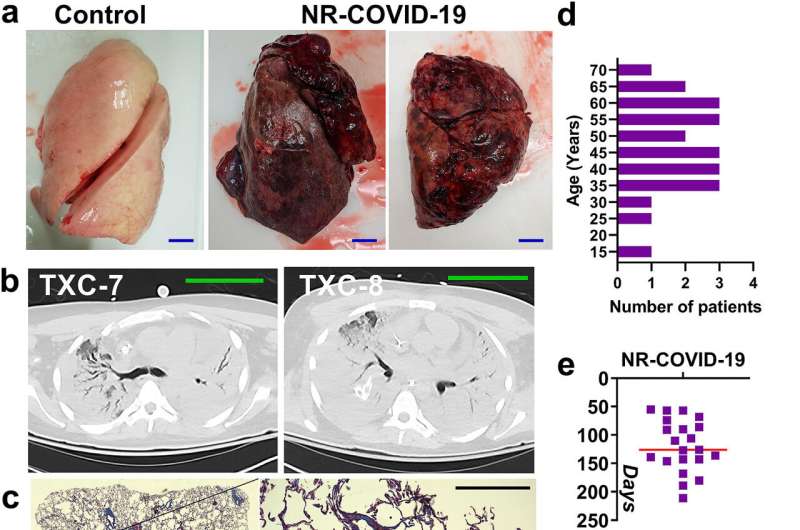
The study looked at 23 patients (19 male and four female) who had non-resolvable COVID-19 and underwent lung transplantation to treat the disease. They had an average age of 47 and included one patient as young as 16.
All the patients underwent lung transplantation between July 2020 and July 2021.
As a control for the study, researchers utilized discarded donor lung tissue and tissue from patients with pulmonary fibrosis of unknown causes. High resolution images demonstrated evidence of extensive fibrosis in the lungs of non-resolvable COIVD-19 patients.
Lung fibrosis progressed rapidly in the COVID-19 positive patients. Within 119 days from the onset of the condition, lung transplantation was required for the patients’ survival.
Typical presentation of pulmonary fibrosis of unknown causes, which is the most common type of cases, can take years to progress into severe lung disease, according to the research. This publication is the one of the handful of studies currently to describe the molecular details of fibrosis in COVID-19 infected lungs.
A different study revealed long-term clinical outcomes of COVID-19 patients who underwent lung transplantation.
The research, published in the September issue of Open Forum Infectious Diseases, found that lung transplantation was an acceptable treatment for lung fibrosis due to COVID-19 infection. A total of 13 patients underwent lung transplantation between January 2020 to March 2022 at Memorial Hermann Hospital in Houston. Of those, six were followed for a minimum of six months after surgery and all but one had little to no post-transplant complications and demonstrated excellent long-term outcomes.
One patient died 218 days after surgery from infectious complications.
The study was led by Hana Javaid, MD, and former transplant infectious diseases fellow at McGovern Medical School, and a team of other researchers from the medical school, including Jyothula.
More information:
Soma S.K. Jyothula et al, Fulminant lung fibrosis in non-resolvable COVID-19 requiring transplantation, eBioMedicine (2022). DOI: 10.1016/j.ebiom.2022.104351
Hana Javaid et al, Post–Lung Transplantation Outcomes and Ex Vivo Histopathological Findings in Severe Post-Covid-19 Pulmonary Disease—A Single-Center Experience, Open Forum Infectious Diseases (2022). DOI: 10.1093/ofid/ofac425
Journal information:
EBioMedicine
Source: Read Full Article


