Researchers have developed an optical biopsy system that can distinguish between cancerous and healthy liver tissue. The new technology could make it easier to diagnose liver cancer, which is the sixth most common cancer globally.
“The instrument is designed to be compatible with the needles currently used for liver biopsies,” said Evgenii Zherebtsov, a member of the research team from Orel State University in Russia. “It could thus one day help surgeons more precisely navigate the biopsy instrument to decrease the number of errors in taking tissue samples that are used for diagnosis.”
In the Optica Publishing Group journal Biomedical Optics Express, the researchers report that the optical biopsy system can reliably distinguish between cancerous and healthy cells in mouse models. The system also showed promise in preliminary tests conducted in people with suspected liver cancer.
“Optical biopsy methods like the one we developed make it possible to differentiate healthy and tumor tissues with a high degree of accuracy,” said Elena V. Potapova, who was co-first author of the paper with Zherebtsov. “Although our system was specifically designed for use in abdominal surgery, our results show that similar technologies could be useful for other medical applications.”
Responding to a clinical need
The researchers designed the new device after the surgeons with whom they were collaborating noted how difficult it is to perform needle biopsies in exactly the right location. Early-stage tumors can be hard to pinpoint when inserting a tiny hollow needle into the liver to acquire a tissue sample. If the needle is placed incorrectly and misses the tumor, it could lead to an incorrect diagnosis.
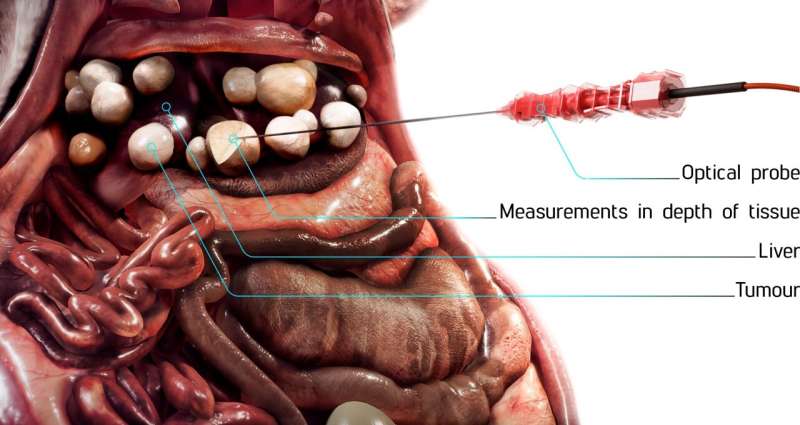
The new optical biopsy system combines diffuse reflectance spectroscopy and lifetime fluorescence measurements to evaluate markers related to cellular metabolism, which differs between healthy and cancerous cells. This could help surgeons see, in real time, where the cancer is so that they can identify the best place to acquire a tissue sample.
Diffuse reflectance spectroscopy reveals tissue properties based on how they reflect light. Fluorescence lifetime analysis exposes tissues to a wavelength of light that induces fluorescence and then measures how long that fluorescence takes to fade. The timing of the fluorescence decay depends on the presence of molecules that are important in metabolism.
“Although our team as well as others have previously used fluorescence intensity for tissue assessment, studies performed in other parts of the body have shown that fluorescence lifetime is less dependent on experimental conditions,” said Potapova. “Fluorescence lifetime measurements remain more consistent in the presence of blood, when there is non-uniform illumination, or if the contact between the probe and tissue changes due to movement.”
With a focus on using the new instrument to guide future biopsies in the clinic, the researchers selected compact, modern components for the device. The 1-millimeter-diameter probe is compatible with a standard 17.5G biopsy needle and has separate optical channels for diffuse reflectance spectroscopy and fluorescence lifetime measurements.

Taking the probe to the clinic
To assess the sensitivity of the assembled system, the researchers first measured known solutions of molecules that play key roles in metabolism. Once they obtained satisfactory results, they then performed experiments in a mouse model with liver cancer and preliminary measurements in patients with suspected liver cancer. The researchers found that their instrument and the parameters they measured could reliably distinguish liver cancer tissue, healthy liver tissue and the metabolically changed liver tissues that surround a tumor.
“It was important to us to compile a comprehensive picture of the observed changes for cancer in both the mouse model and the clinical setting,” said Zherebtsov. “Our studies in patients who had the same type of tumor as the mice showed that our technique can provide stable, reproducible results that can be used to detect cancer.”
Source: Read Full Article


