Researchers say newly reported cases of cancer diagnoses declined 14.4% in 2020 compared with prior years, correlating with the timing of stay-at-home orders in the early months of the COVID-19 pandemic.
A new study, based on reported cases of new cancer diagnosis to the National Cancer Database (NCDB), estimates roughly 200,000 people with cancer cases weren’t diagnosed or treated at Commission on Cancer-accredited facilities at the onset of the pandemic in 2020, around the same time that triage guidelines recommended delays in cancer-related care.
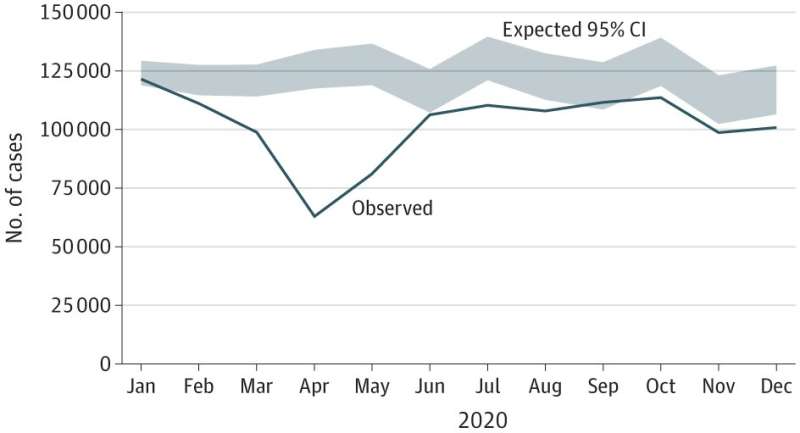
The study’s lead author said analysis showed an overall trend of cancer cases dropping off in March 2020 and reaching an ultimate low in April before a partial recovery mid-year. However, there was no rebound of backlogged cases or return to case levels seen in prior years.
“Our findings revealed what we all feared, that many cancer cases didn’t come in during the early pandemic and didn’t catch up during that first year, meaning those ‘missing cases’ are out there somewhere,” said Sharon Lum, MD, MBA, chair of the Loma Linda University Health Department of Surgery and the study’s principal investigator. “Our concern is that these patients may show up later, potentially at more advanced disease stages.”
The study was published today in JAMA Surgery. Its authors hope their findings will serve as a reference for those utilizing NCBD data to conduct research, quality reports, and process improvement projects.
Lum said researchers wanted to alert those using NCBD data from 2020 that all of their reports are going to be altered in some fashion from the disruption in reported cases.
The NCDB, a joint project by the American College of Surgeons Commission on Cancer and the American Cancer Society, is one of the largest cancer registries in the world, representing more than 70% of all cancer cases in the United States. Nearly 1,500 programs accredited by the Commission on Cancer, including Loma Linda University Health, leverage NCBD data to improve the quality of cancer care in the United States, Lum said. She previously served as vice-chair of the Commission on Cancer’s quality integration committee.
Year over year since 1989, NCDB data have proven historically reliably stable, Lum says. Yet “the COVID-19 pandemic destabilized usual patterns of cancer care,” the study authors wrote.
Lum and researchers from academic and medical institutions across the nation examined all cancer cases added to the NCDB in the years leading up to the pandemic and analyzed the variances in reported cases during 2020 compared to 2018 and 2019. Their research revealed that the monthly decline in cancer cases logged in the NCDB during 2020 correlated with the timing of stay-at-home orders and triage guidelines recommending intentional delays in cancer-related care.
Additionally, Lum says researchers observed smaller-than-expected numbers of early-stage diseases in the pandemic’s early months and simultaneously observed more than expected cases of late-stage diseases.
Researchers did not identify any overall patterns in patient demographics to account for the varied differences of observed-to-expected proportions of reported cancer cases, Lum says.
“The differences in expected versus observed cases didn’t happen in the same way across the board for every single cancer site,” Lum says. “There were high levels of variation between different diseases and individual cancer sites.”
The study’s findings provide month-by-month breakdowns of NCDB’s 2020 trends in reported cases, Lum says; the monthly analysis isn’t standardly available to NCDB users and offers valuable insights into details of the year’s progression. The findings call for NCDB users engaged in cancer care quality reporting, process improvement, or research to carefully interpret disease- and program-specific results for 2020 and years to come to account for the disrupted pandemic year data. Study authors recommend users perform their own validation studies before incorporating 2020 data and use disclaimer language in publications using 2020 NCDB data.
“We are alerting the cancer community to look carefully at their institutional data to see how what happened in 2020 could have affected what their reports looked like,” Lum said. “Database users should consider what activities took place in their local and institutional environment that first year of the pandemic.”
Lum said the downstream effects of the 2020 data set, such as impacts on longitudinal survival reports, have yet to be understood. The Commission on Cancer will follow the 2020 NCDB cohort and conduct similar validity studies with the subsequent data cohorts in 2021 and 2022. Future research can also evaluate COVID-19 infection-related associations, treatment adherence and outcomes, and long-term follow-up of the 14.4% of cancer diagnoses that were not treated as expected in Commission on Cancer-accredited cancer programs.
More information:
Sharon S. Lum et al, Disruption of National Cancer Database Data Models in the First Year of the COVID-19 Pandemic, JAMA Surgery (2023). DOI: 10.1001/jamasurg.2023.0652
Journal information:
JAMA Surgery
Source: Read Full Article


