What scientists learned about the rare antibodies targeting SARS-CoV-2’s Achilles’ heel could help fine-tune our COVID-19 vaccine strategy for longer-lasting immunity.
New research examining how frequently our bodies produce broadly neutralizing antibodies (bnAbs) capable of thwarting a range of SARS-CoV-2 variants offers clues on the strategy tweaks that could potentially future-proof COVID-19 vaccines.
To counter invading viruses, our body deploys specific antibodies, among them the neutralizing type that targets the receptor-binding domain (RBD)—the “Velcro hooks” used by pathogens to fasten onto our cells. As SARS-CoV-2 accumulates genetic mutations, new variants emerge donning sneaky disguises to outsmart our defenses. So-called bnAbs are elite neutralizing antibodies that can keep up with the virus’ evolving tricks. Unfortunately, conventional COVID-19 vaccines have struggled to elicit them.
“Conventional COVID-19 vaccines are known to be less effective against emerging SARS-CoV-2 variants due to the difficulty in producing bnAbs,” said study corresponding author Tomoharu Yasuda, professor at Hiroshima University’s (HU) Graduate School of Biomedical and Health Sciences.
“In order to develop a vaccine with sustained efficacy, it is important to clarify the mechanisms of how bnAbs are generated after virus infection.”
The study by HU, Kyoto University, and Hiroshima Prefectural Hospital researchers was published in the journal Communications Biology in April.
Examining bnAbs
Observing blood sera at 8–55 days from 18 unvaccinated patients in their first bouts of COVID-19, the researchers noticed a surge in neutralizing antibodies in samples starting 17 days following diagnosis. As hospitalizations dragged on, they found that sera collected on the 55th day outperformed the rest, exhibiting the highest frequency of bnAbs compared to those taken at other time points.
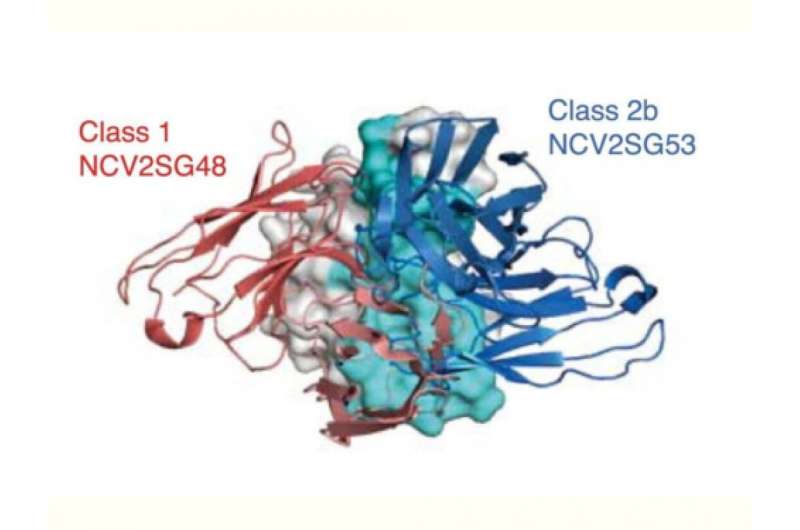
Analyzing the samples, the researchers identified four therapeutic monoclonal antibody (mAb) candidates—NCV1SG17, NCV1SG23, NCV2SG48, and NCV2SG53—that neutralized the authentic SARS-CoV-2 strain infecting the patients. All study participants were long-term cases infected with an earlier B.1.1 strain of the novel coronavirus containing the D614G spike mutation believed to enhance viral infectivity. The four mAbs also took out the original SARS-CoV-2 virus strain (Wuhan-Hu-1), alpha, delta, and variants with point mutations only at K417, L452, or E484 known to decrease sensitivity to antibody neutralization.
All, however, failed to neutralize omicron BA.1 except for NCV2SG48, which showed equivalent potency against the variant as Sotrovimab, among the few mAbs treatments that work against this omicron sublineage. NCV2SG48 also warded off omicron BA.2 and BA.4/5.
Upon closer investigation into what makes it so potent, the researchers found that prolonged exposure for nearly two months to SARS-CoV-2 triggered the patients’ germinal centers (GC) to introduce a high rate of changes called somatic hypermutations (SHMs), equipping NCV2SG48 with an extensive binding interface.
NCV2SG48 specifically targets conserved residues in the receptor-binding motif (RBM)—an RBD subdomain that directly interacts with the cell’s ACE2, the “loops” that the virus latches on for entry. These conserved residues tend to remain unchanged across variants as they can’t tolerate mutations without affecting the pathogen’s ability to infect and replicate. Given its key part in cell entry and the evolutionary pressure to keep areas tied to this role unaltered in future versions, the RBM is an attractive Achilles’ heel for bnAbs to attack. NCV2SG48 has taken advantage of this coronavirus region’s vulnerability.
Its immense binding interface allowed NCV2SG48 to block not only its targeted conserved residues but the neighboring amino acids as well, effectively covering almost the entire virus surface interacting with ACE2. Imagine it like a clump of lint whose strands are sticking out in every direction obstructing the pathogen’s “Velcro hooks.” When reverted to its original version, NCV2SG48 performed poorly in warding off the alpha, beta, omicron BA.1, BA.2, BA.2.12.1, and BA.4/5 variants, affirming the critical role of SHMs in its potency.
Clues to longer-lasting COVID-19 vaccines
The researchers also found that NCV2SG53, another bnAb that gained new interaction sites due to SHMs, works well with NCV2SG48. A cocktail made of these two antibodies broadly neutralized variants at low concentrations showing promise as a COVID-19 treatment, especially as a pre-exposure drug for the immunocompromised.
“We found that bnAbs are created by amino acid substitutions, called somatic hypermutation, in the antigen recognition site of antibodies. It produced additional binding sites and markedly extended the binding interface between the antibody and the viral receptor, which contributed to the neutralization of broad variants,” Yasuda explained.
He believes their findings could help refine our vaccination strategy to mimic sustained exposure of about two months.
“We do not need to develop a completely new vaccine to induce bnAbs,” he said. “A single vaccine shot generally maintains 2–3 weeks of germinal center reaction. So by getting a general vaccine three times, the duration of GC reaction could be around two months in total.”
By switching antigens from different SARS-CoV-2 variants one after the other during GC reaction, Yasuda said vaccines could induce a response similar to what occurs during chronic infection, where viruses continuously mutate as they replicate, but sans the obvious symptoms.
“We previously showed that antigenic shift immunization approach enhances bnAbs,” he said, referring to a previous study the current authors were also involved in suggesting that an omicron booster elevates bnAbs levels in individuals earlier vaccinated with the original SARS-CoV-2 antigen.
The researchers have now started discussions on developing an mRNA vaccine that is capable of inducing bnAbs based on their findings.
“We hope that our findings contribute to the development of effective vaccines and therapeutics against other pandemics and bioterrorism.”
More information:
Kiyomi Shitaoka et al, Structural basis of spike RBM-specific human antibodies counteracting broad SARS-CoV-2 variants, Communications Biology (2023). DOI: 10.1038/s42003-023-04782-6
Journal information:
Communications Biology
Source: Read Full Article


