In a new study from INSPIRE (Innovative Support for Patients with SARS-CoV-2 Infections Registry), researchers compared new and ongoing symptoms and outcomes in both COVID-positive and COVID-negative adults who were tested because of acute COVID-19-like symptoms. The study found that half of the patients with COVID-19 and one-quarter of those who tested negative had at least one symptom at three months follow-up.
The CDC defines symptoms of COVID-19 persisting beyond four weeks as “long COVID.” Due to its extensive range of symptoms, the post-viral syndrome is challenging to research and is poorly understood. This study, in which Yale New Haven Health was one of eight health care systems that participated, was published in Clinical Infectious Diseases on December 27 and is part of the larger INSPIRE, a CDC-funded registry. The study will be one in a series of INSPIRE research efforts dedicated to better understanding the lasting impacts of SARS-CoV-2 infection.
“These data are important for driving research and policy, but also for bringing light to people’s experiences,” says Erica Spatz, MD, associate professor of cardiology and of epidemiology (chronic diseases) at Yale, and one of the first authors. “It’s validating for patients who are experiencing long COVID, and a message to clinicians that this is common and to be prepared to take care of people with this condition.”
Collaborating to study poorly understood long COVID
Studies on the prevalence of long COVID post-infection vary considerably—from 10% to as high as 65%. This variability, says Spatz, is due to differences in methodology, including who participated in the studies, the length of follow-up, and the comprehensiveness of symptoms studied. For instance, long COVID can manifest in many ways—it can alter a patient’s neurocognitive, cardiovascular, pulmonary, musculoskeletal, and psychological health. This makes the condition difficult to characterize.
“Through my own personal experience taking care of patients with long COVID, as well as what is described in the literature, we know that the symptoms span every organ system,” she says. “And so we need to be really comprehensive in evaluating people’s symptoms to allow us to understand the multitude of different sequelae that could occur.”
As a cardiologist and researcher focused on cardiovascular disease prevention, in 2020 Spatz says she found herself “in a world of long COVID” as she took care of hundreds of patients as part of a multidisciplinary care team at Yale. This sparked her interest in the post-viral syndrome, so she and others both within and outside of Yale responded to CDC’s broad agency announcement for research to understand the ongoing effects of COVID-19. The contract CDC awarded enabled them to conduct longitudinal cohort studies and observe the experiences of individuals who contracted SARS-CoV-2 over 18 months.
The team enrolled individuals from eight sites around the country, including Yale New Haven Health, RUSH University Medical Center, and University of Washington. To find potential participants, they reached out to nearby hospitals, emergency departments, testing centers, and community health clinics to identify people who had recently taken a COVID-19 test. They enrolled any participant who was experiencing symptoms at the time of taking the test. Those who tested negative were used as the control group.
“What’s novel about our study is that we follow people from the time that they get tested.” says Spatz. “So we have a control cohort and can compare the experiences of people with and without COVID-19 from a common starting point.”
After enrollment, participants took a baseline survey and shared their medical records through Hugo Health, a company started by Harlan Krumholz, MD, Harold H. Hines, Jr. Professor of Medicine (Cardiology). Every three months, for 18 months, the team sent participants surveys that evaluated the range of symptoms they may be experiencing.
“Beyond the unique focus on long COVID, the INSPIRE registry reflects an entirely new way of doing research,” says Arjun Venkatesh, MD, incoming chair and associate professor and chief of the section of administration in the Department of Emergency Medicine, who also contributed to the latest publication as one of its senior authors. “While the COVID-19 pandemic upended traditional research, INSPIRE reflects Yale’s innovative approach to research on which the majority of participants have been enrolled virtually and most have shared data through an entirely digital mobile platform.”
COVID-19 symptoms frequently linger
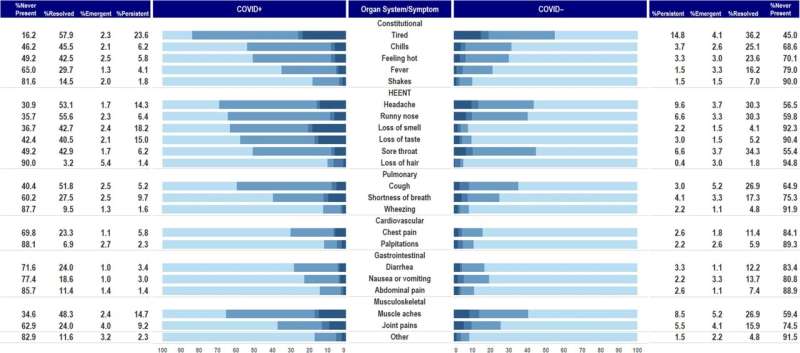
In their recently published study, the team evaluated long COVID in the first 1,000 enrollees. At the three-month mark, they found that persistent or newly emergent symptoms were common. Nearly half of those in the COVID-19 positive group were experiencing at least one symptom, as well as about a quarter of those in the COVID-19 negative group. Interestingly, fatigue symptoms—level of exhaustion post-physical or mental exertion, quality of sleep, or generalized muscle aches and pains—were similar across both groups. One in six people across both groups experienced severe fatigue.
“This is a clue that there are a lot of other people struggling,” says Spatz. “Chronic fatigue is common after other infectious diseases, too. We’re also all living through this pandemic. There are many different stressors that may be resulting in these systemic symptoms.”
The publication, Spatz says, will be one of many on long COVID and its impact. INSPIRE has enrolled 6,000 participants, and the team plans on using the registry to look at long-term health outcomes, including whether they differ based on SARS-CoV-2 variant period or COVID-19 vaccination status, whether essential workers were differentially affected, the number of people returning to work, and more. One such paper was published January 27. “These are really important data that may inform policy, including absenteeism and family medical leave and disability, as well as research into mechanisms and treatment,” says Spatz.
More information:
Erica S Spatz et al, Three-Month Symptom Profiles Among Symptomatic Adults With Positive and Negative Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Tests: A Prospective Cohort Study From the INSPIRE Group, Clinical Infectious Diseases (2022). DOI: 10.1093/cid/ciac966
Journal information:
Clinical Infectious Diseases
Source: Read Full Article