Acute kidney injury (AKI) is a clinical syndrome characterized by a decrease in kidney function. AKI is very common in the United States’ Medicare population, particularly among hospital intensive care unit (ICU) admissions. Furthermore, AKI is associated with the incidence of end-stage renal disease, which eventually increases the burden of long-term care, higher health-care costs, and increased mortality.
In several instances, kidney diseases have been linked to air pollution exposure. Inhaling air pollutants, including gases like nitrogen dioxide (NO2), ozone (O3), and fine particulate matter (PM2.5) that remains suspended in the air, can cause a decrease in kidney function, damaging the tissues and increasing the risk of AKI.
Long-term exposure to these pollutants has been linked to DNA damage in renal tissue sepsis, which ultimately leads to AKI. However, studies on the effects of environmental stressors such as air pollution on AKI are lacking.
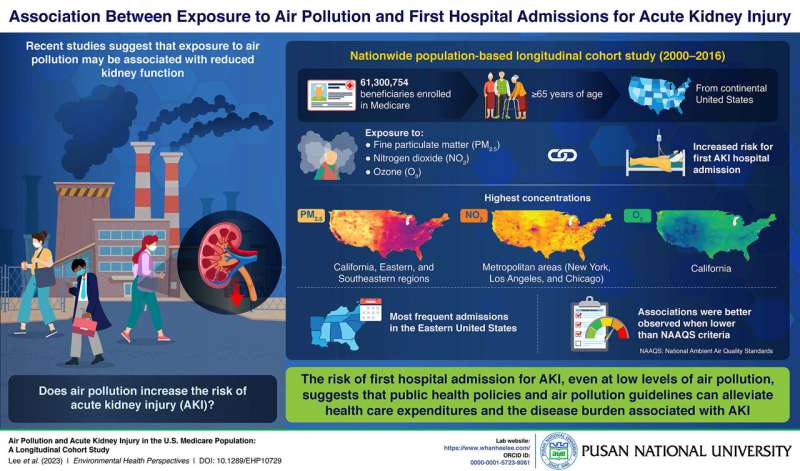
To address this gap in research, a team of scientists, including Assistant Professor Whanhee Lee from Pusan National University, performed a population-based study to find out if increased air pollution exposure was responsible for the first hospital admissions of patients with AKI in the United States.
“Our study investigated the association between air pollution and first hospital admission for AKI using a national retrospective cohort of more than 61 million Medicare beneficiaries. It provides scientific evidence that the public health benefits of stricter air pollution standards may alleviate the risk of AKI,” says Prof. Lee. Their findings were made available in Environmental Health Perspectives.
The team analyzed data for over 61 million patients (aged >65 years) who lived in the continental United States from 2000 through 2016 and were enrolled to receive support from Medicare. Their findings confirmed that exposure to PM2.5, NO2, and O3 was associated with an increased risk of first hospital admission for AKI. Interestingly, this association existed even at annual exposures lower than the current National Ambient Air Quality Standard.
Moreover, older adults (>75 years), White people, and those not eligible for Medicare, were found to be more affected by air pollution. The most frequent first hospital admissions for AKI were recorded in the southeastern region, which had the highest levels of PM2.5. In contrast, metropolitan areas such as New York, Los Angeles, and Chicago had the highest levels of NO2, while California had the highest O3 concentration. These data are certainly concerning from the standpoint of public health.
Prof. Lee explains, “Our findings suggest beneficial implications for public health policies to alleviate healthcare expenditures and disease burden attributable to AKI and also provide epidemiological evidence on the value of air pollution guidelines for potential AKI patients.”
The findings of this study could be influenced by the potential confounding effects of underlying health conditions. However, they certainly help “clear the air” on the association between kidney disease and air pollution.
More information:
Whanhee Lee et al, Air Pollution and Acute Kidney Injury in the U.S. Medicare Population: A Longitudinal Cohort Study, Environmental Health Perspectives (2023). DOI: 10.1289/EHP10729
Journal information:
Environmental Health Perspectives
Source: Read Full Article


