Changing the order of treatments given to breast cancer patients could reduce side effects and improve outcomes, according to an Imperial study.
In a clinical feasibility trial, published in The Lancet Oncology, researchers found that switching the sequence of treatments given to breast cancer patients was safe, without any increase in complications and could lead to patients receiving faster and more effective care compared to current methods.
Thirty-three women with breast cancer requiring a mastectomy—an operation to remove a breast or breasts to treat cancer—and post-mastectomy radiotherapy, were recruited to the primary radiotherapy and deep inferior epigastric perforator flap reconstruction for patients with breast cancer (PRADA) trial between January 2016 and December 2017. They were also eligible for a breast reconstruction using tissue from another part of their body.
They were given chemotherapy followed by radiotherapy before having a mastectomy and a breast reconstruction. The team found that this approach was feasible and safe. They also found that side effects were low and that 12 months after surgery patients reported high levels of satisfaction with their breast reconstruction.
The study was led by researchers at Imperial College London and clinicians at The Royal Marsden NHS Foundation Trust and Imperial College Healthcare NHS Trust. It was funded by the National Institute for Health and Care Research Imperial Biomedical Research Center (BRC) and the Cancer Research U.K. (CRUK) Imperial Center.
It is the first multi-center study to provide comprehensive data on the surgical safety, treatment pathway times, and aesthetic outcome of this new treatment approach.
Maxine Myers caught up with the lead authors of the study: Daniel Leff, Reader in Breast Surgery in the Department of Surgery & Cancer and Honorary Consultant in Oncoplastic Breast Surgery at Imperial College Healthcare NHS Trust, and Paul Thiruchelvam, Honorary Clinical Senior Lecturer in Breast Surgery at Imperial College London and a Consultant Surgeon at Imperial College Healthcare NHS Trust, to find out more about this research.
Can you tell me about your study?
Daniel Leff (DL): The research we are undertaking seeks to tackle major issues associated with reconstructive surgery, following a mastectomy and radiotherapy for breast cancer patients.
Many breast cancer patients who need a mastectomy will also desire a reconstruction and require radiotherapy. Internationally, many hospitals will only offer patients a mastectomy first followed by radiotherapy and then reconstruction at a later date, meaning many women will have to wait for a reconstruction, which can often be delayed by many years. Some women will not receive delayed reconstruction at all.
Other hospitals decide to proceed with reconstruction at the time of mastectomy and then give radiotherapy to the chest wall (including to the reconstruction itself). However, this pathway can lead to complications such as damage to healthy tissues used to do the reconstruction—including shrinkage, firmness and loss of symmetry.
We wanted to see whether changing the sequence of treatments was safe in the short term and would reduce these complications in the long term.
Can you explain more about the complications some patients experience following radiotherapy to breast reconstructions?
DL: The type of complications we see are shrinkage and loss of symmetry in the reconstructed breasts. Some women also experience a firm hard lump in their breast following radiation called “fat necrosis”—a non-cancerous condition that can develop when an area of fatty breast tissue is injured.
This occurs because the radiation used to kill cancer cells can impair the blood supply to certain areas of the reconstruction causing a palpable lump. As these patients have been through breast cancer, feeling a lump in your reconstructed breast can cause significant worry and anxiety even if it is non-cancerous.
Additionally, there is evidence suggesting that patients who have radiation after surgery have a worse quality of life in terms of satisfaction with their reconstruction and physical health due to these complications.
What were the main findings of the study?
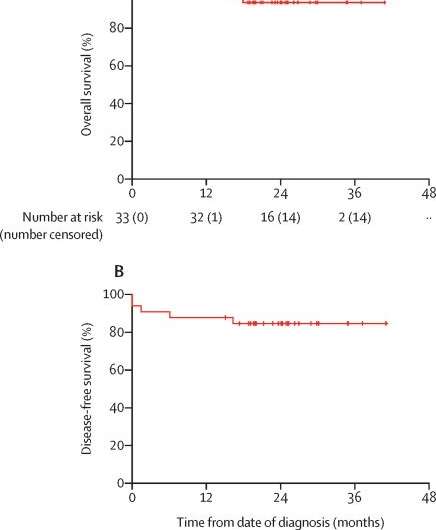
DL: We recruited 33 patients to the study and found that changing the sequence of the treatment was safe and technically feasible. The rates of complications were similar to those reported in other studies—four patients developed an open wound greater than one centimeter and one patient had required a re-operation to tackle dead skin.
We also surveyed patients three months and 12 months after surgery on their breast reconstructions and found a high level of patient satisfaction with a satisfaction score of 77% and none of the patients’ cancers returned in or around the reconstructed breast 12 months after treatment.
How significant are these findings?
Paul Thiruchelvam (PT): Approximately 55,000 women and 370 men are diagnosed with breast cancer every year in the U.K., so these findings are hugely significant because it means we now have evidence that shows giving patients radiation therapy before a mastectomy and a reconstruction is safe.
Specifically, our results demonstrate that radiation therapy did not impact the ability of surgeons to perform complex breast reconstructions such as using tummy tissue to create a new breast mound that comes as close as possible to the form and appearance of the natural breast or breasts.
Also, there was no increase in the frequency of problems we see after breast surgery such as infections of the wound, necrosis (death of body tissue) of the mastectomy skin or with the reconstruction failing to pick up a blood supply. Finally, none of the patients’ reconstructions failed (i.e., had to be removed).
How can this study benefit the NHS?
PT: The study could benefit the NHS in several ways. Firstly, compared to standard care, our treatment approach may reduce the overall treatment journey for patients by approximately one month.
We believe that, in the long term, this approach will improve patients’ mental and physical well-being with higher quality of life scores and satisfaction with their reconstructed breasts compared to current care. It also means that many patients who are currently denied reconstruction due to concerns of further complications due to radiotherapy may be able to get access to this treatment in future.
What are the next steps?
Source: Read Full Article


