In a remarkable breakthrough, a collaborative team of researchers, led by Professor Yaakov Nahmias from The Hebrew University of Jerusalem, Technion-Israel Institute of Technology, and Tissue Dynamics Ltd., has unveiled a miniature human heart model that could potentially transform drug testing and cardiovascular research.
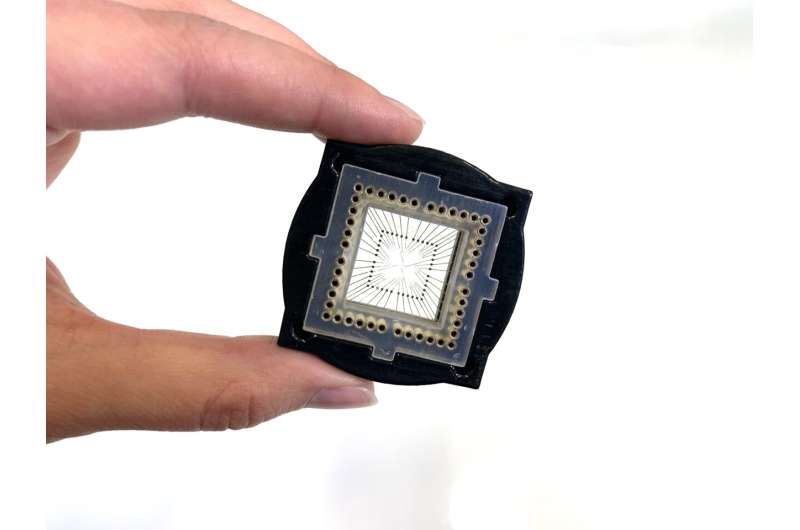
This study, published in Nature Biomedical Engineering, introduces a self-paced multi-chambered human heart model, no larger than a grain of rice, which promises to revolutionize the way we study the heart and its functions.
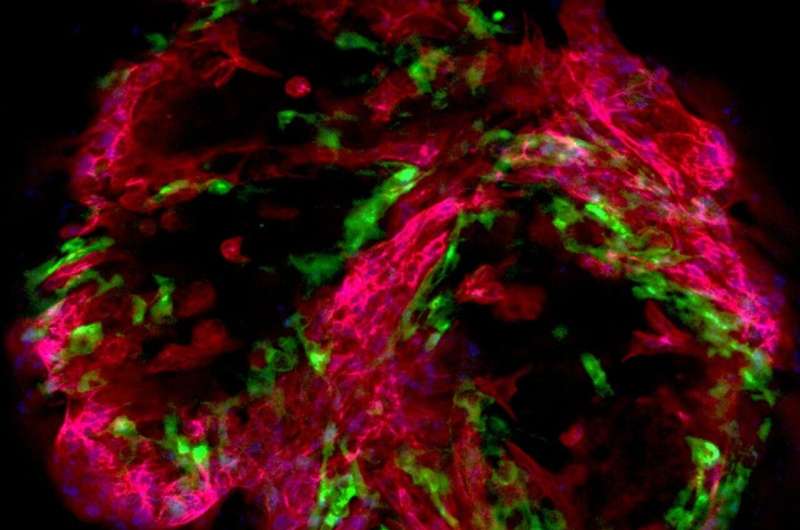
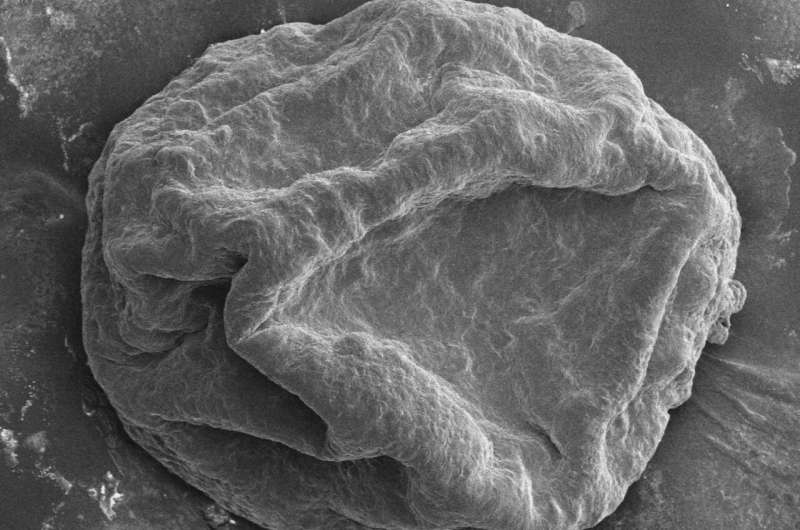
Cardiovascular diseases remain the leading cause of global mortality, underscoring the critical importance of this pioneering work. Professor Nahmias and his team embarked on an intricate endeavor to create an accurate replica of the human heart using human induced pluripotent stem cells (hiPSCs). The resulting model comprises multiple chambers, pacemaker clusters, epicardial membrane and endocardial lining, all meticulously designed to mimic the structure and functions of the human heart.
One of the most significant features of this heart model is its ability to provide real-time measurements of essential parameters such as oxygen consumption, extracellular field potential, and cardiac contraction. This capability enabled the scientists to gain unprecedented insights into heart function and diseases, making it a game-changer in the field of cardiovascular research.
The heart model, approximately the size of half a grain of rice, represents a remarkable feat in cardiac research and holds immense potential for precision drug testing. Already, the research team has made groundbreaking discoveries that were previously unattainable using conventional methods. Notably, the heart model unveiled a new form of cardiac arrhythmia, distinct from those observed in traditional animal models, thereby offering new avenues for studying human physiology.
The implications of this discovery extend to the pharmaceutical industry, as it allows researchers to gain invaluable insights into the precise effects of pharmaceutical compounds on the human heart. The heart model’s response to the chemotherapeutic drug mitoxantrone, commonly used to treat leukemia and multiple sclerosis, was carefully tested.
Through these experiments, the researchers pinpointed how mitoxantrone induces arrhythmia by disrupting the heart’s electro-mitochondrial coupling. Encouragingly, the team also discovered a potential solution by administering metformin, which showed promise in mitigating the drug’s adverse effects.
Professor Nahmias, Director of the Grass Center for Bioengineering at The Hebrew University of Jerusalem and a fellow of the Royal Society of Medicine and AIMBE, emphasized the significance of their work. “The integration of our complex human heart model with sensors, allowed us to monitor critical physiological parameters in real-time, revealing intricate mitochondrial dynamics driving cardiac rhythms. It is a new chapter in human physiology,” said Nahmias.
Partnering with Tissue Dynamics, the scientists developed a robotic system that can screen 20,000 tiny human hearts in parallel for drug discovery applications. The potential applications of this micro-physiological system are vast, promising to enhance our understanding of heart physiology and accelerate the discovery of safer and more effective pharmaceutical interventions, leading to a healthier future for all.
By offering unparalleled accuracy and insights into cardiovascular diseases, this advanced human heart model has the potential to revolutionize drug testing methodologies. With this tiny heart model, researchers are poised to make significant strides in developing safer and more effective medications for patients worldwide, potentially saving lives and improving patient outcomes.
Moreover, the miniature heart model also presents an ethical advantage, as it offers a viable alternative to animal testing. This breakthrough discovery could mark a turning point in the pharmaceutical industry, reducing reliance on animal models and minimizing potential harm to animals in the pursuit of medical advancements.
In conclusion, the tiny heart model developed by Professor Nahmias and his team represents a monumental achievement with far-reaching implications for medical research. This miniature yet sophisticated human heart model has the potential to reshape drug testing practices, advance our understanding of cardiovascular diseases, and ultimately contribute to a healthier and more sustainable future.
More information:
Yaakov Nahmias et al, Electro-metabolic coupling in multi-chambered vascularized human cardiac organoids, Nature Biomedical Engineering (2023). DOI: 10.1038/s41551-023-01071-9
Journal information:
Nature Biomedical Engineering
Source: Read Full Article


