A new distributional cost-effectiveness analysis of gene therapy versus standard-of-care for sickle cell disease (SCD) found that while gene therapy is cost-ineffective by conventional measures, it can be an equitable therapeutic strategy for persons living with SCD in the United States when equity, cost, and value of treatment are considered together.
These findings highlight systemic health inequities faced by persons with sickle cell disease (SCD). The authors say this is the first quantitative consideration of health equity for patients with SCD regarding the decision between gene therapy and standard care and the first study of its kind in any rare disease. The analysis is published in Annals of Internal Medicine.
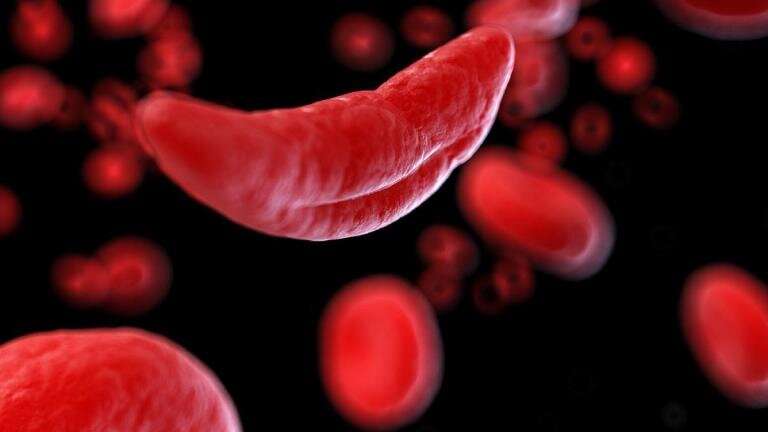
Persons with SCD face substantial mortality risks and decreased quality of life for every year they live with the disease. SCD occurs more often in people whose ancestors came from sub-Saharan Africa and other parts of the world where malaria is or was common. In the United States, this means that patients are predominantly drawn from socially disadvantaged ethnic minority populations. Gene therapy treatment would allow for lifelong disease remission without the concomitant risks associated with allo-transplantation, but it is prohibitively expensive.
Researchers from Yale University School of Medicine studied claims data and other published sources to compare gene therapy versus standard-of-care in patients with SCD by using conventional cost-effectiveness and distributional cost-effectiveness measures.
While conventional cost-effectiveness analysis does not capture the effects of treatments on disparities, distributional cost-effectiveness uses equity weights to incorporate these considerations. The authors found that the total quality-adjusted life years, or QALYs, for persons receiving gene therapy treatment for SCD would cost $2.8 million versus $1.2 million for persons receiving standard care.
According to the authors, the inequality aversion parameter would need to be 0.90 for the full SCD population for gene therapy to be preferred per distributional cost-effectiveness standards. This is right in line with benchmark values previously reported in the United States for inequality aversion (range: 0.5-3.0), with higher values representing a higher emphasis on reducing a particular health disparity.
An accompanying editorial from the Centre for Health Economics, University of York; York, United Kingdom highlights that the results of this analysis do not provide a simple answer to how much U.S. healthcare payers should be willing to pay for increasing health equity, but it does provide quantitative information that can help facilitate transparent and consistent decision making.
The author argues that to help reduce health disparities, health care payers need to invest more in equity-enhancing technologies for conditions that disproportionately affect socially disadvantaged populations and are often underdiagnosed and poorly managed in such populations.
More information:
Study: Annals of Internal Medicine (2023), DOI: 10.7326/M22-3272. www.acpjournals.org/doi/10.7326/M22-3272
Editorial: Annals of Internal Medicine (2023), DOI: 10.7326/M23-1145. www.acpjournals.org/doi/10.7326/M23-1145
Journal information:
Annals of Internal Medicine
Source: Read Full Article


