Despite COVID’s retreat, it seems that many of us are still getting sick, even before flu season has arrived. Rates of influenza-like illnesses, Strep, tonsillitis, the common cold – and for many, that’s been an absolute monster cold – have all been on the rise. One explanation put forward by experts has been the “immunity debt”, whereby two years of lockdown and social distancing limited our exposure to pathogens and left us more susceptible.
“Everything starts to go wrong with age, like a car with wear and tear, but the immune system is particularly susceptible to age-related decline,” says Dr Jenna Macciochi.Credit:iStock
So if you’re always getting sick and wondering if your immune system is up to scratch, is there any way of measuring it? Blood tests can look at inflammatory molecules and numbers of immune cells, and a more sophisticated test recently developed in America now classifies your “immune grade” by looking at the T-cell balance – specifically the ratio of “helper T-cells”, which sense infection, to “killer T-cells” that can destroy infected cells.
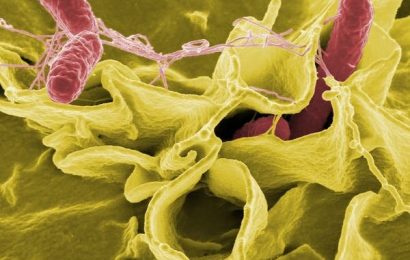
However, our immune system has multiple components, including our skin, airways, microbiome and mucus membranes. It’s an army with units all over the body, patrolling for bugs, attacking and “peacekeeping” – signalling that the war is over and mopping up the damage. (The peacekeepers are essential because an overly aggressive immune system creates autoimmune diseases, where the body turns on itself.)
As yet, we don’t have good tools or a single test to measure all this, but until we do perhaps the easiest way to tell if your immune system is up to scratch is by how often you get sick. “As a general guide, a healthy adult can expect between two and four minor illnesses each year,” says immunologist Dr Jenna Macciochi, author of Your Blueprint for Strong Immunity. “If you’re suffering more than that, or, more importantly, you’re noticing different patterns and symptoms, more unusual infections, or you’re not recovering well, you may want to see your GP.”
When it comes to strengthening your immune system, much is beyond your control. “It’s down to a messy mixture which includes your genetics, past illnesses and what you’ve already been exposed to,” says Macciochi. Age also counts.
“Everything starts to go wrong with age, like a car with wear and tear, but the immune system is particularly susceptible to age-related decline.” So what can we do to make a difference?
Feed your microbiome
“One of the most important factors is good gut health since a significant proportion of your immune system – approximately 70 per cent of the body’s immune cells – are located in your gut,” says Kate Llewellyn-Waters, nutritionist and author of The Immunity Cookbook. The trillions of bacteria located here – known as the gut microbiome – play a role in training immune cells, triggering immune responses or dampening them down. The more diverse the microbiome, the broader that education will be. “It’s important to make sure our guts have as many different bacteria species as possible by eating a wide variety of different foods.”
Focus on prebiotic and probiotic-rich foods, advises Llewellyn-Waters. Prebiotic-rich foods include apples, asparagus, artichokes, bananas, broccoli, cauliflower, fennel, garlic, legumes, leeks, onions, bok choy, wheat and oats. Probiotics, important for their live microbes, are fermented foods, like sauerkraut, fermented tempeh, miso, kefir and live natural yoghurt.
Keep blood sugars stable by avoiding sugary, ultra-processed foods and following a consistent meal schedule which includes protein. Elevated blood sugars weaken our antiviral defences and promote viral replication. One 2021 study found it the most likely risk factor to explain why otherwise healthy patients get severe COVID-19.
Should we take a vitamin supplement? “Some of the key vitamins and minerals involved in supporting our immunity include vitamins A, C, D, E as well as the B-vitamins and the minerals zinc and selenium,” says Llewellyn-Waters. “For most people I’d advise focusing on getting your nutrients from your diet first, although one supplement I often recommend for people over 60 is vitamin B12, since this micronutrient becomes harder to absorb as we age. If you are elderly, or under a lot of physical or emotional stress, you may wish to consider an all-round, high-quality multivitamin supplement.”
The only vitamin supplement that immunologist Dr Jenna Macciochi takes is Vitamin D. “We’re probably not going to get sufficient quantities from our diet and there is insufficient sunlight in [winter to boost your Vitamin D supply],” she says.
Harness your body clock
It isn’t just getting enough sleep that’s important to immunity – it’s when you do it. The circadian system regulates every aspect of our immune system, right down to our skin, which becomes more permeable at night, drier, itchier and with less defence against pathogens entering the body. “The immune system is turned up in daytime, but it begins to be turned down as you approach late afternoon and at night it’s low,” says Russell Foster, professor of circadian neuroscience at the University of Oxford and author of Life Time.
A cut or a burn will heal more than twice as fast if it occurs during the day rather than at night. One explanation for all this is that running permanently on full throttle raises the risk of autoimmune disease – and also requires huge energy – so our immune system is primed for daytime, when we should be most likely to need it.
A growing body of evidence is showing that living in harmony with the circadian system is essential for optimal immunity. One study looked at antibody response to flu vaccinations and found it threefold greater in those vaccinated in the morning compared with those vaccinated in the late afternoon – so schedule yours accordingly. Another study found that the activity of natural killer (NK) cells – critical for immunity – fell by an alarming 28 per cent in healthy males when they had been deprived of sleep between 3am and 7am.
Regular all-nighters play havoc with immunity – night shift workers were more likely to be admitted to hospital with COVID. “Your entire biology is working when you should be asleep, and that activates the stress axis, elevates cortisol levels and acts as an immunosuppressant,” says Foster.
“When it comes to scheduling your sleep, there’s no one size fits all,” adds Foster whose book includes a section on how to work out your own optimal sleep pattern for immunity and health. “It might be six hours, it might be 10 hours, it changes as we get older, but the important thing is to defend it and realise what you can get out of it. It’s not an expendable luxury.”
Keep moving
Sitting at your desk all day then spending an hour at the gym won’t cut it, says Macciochi. “It’s ‘movement’, rather than exercise that’s important. Sitting all day is an independent risk factor for the immune system.” Our lymphatic fluids, which carry immune cells around the body, have no pump to make them flow – they need our muscles to be moving.
Muscle activity also produces molecules which act on the thymus gland where T-cells are produced. One UK study of 125 adults aged between 55 and 79 who had maintained a high level of activity (cycling) through much of their adult life showed their immunity as measured in T-cells still matched those of young adults.
A review of 16 studies representing two million adults in 10 countries found that people who stayed physically active through the pandemic – despite lockdown rules and the closure of sports clubs and fitness spaces – had a 36 per cent lower risk of hospitalisation from COVID-19 than those who were more sedentary. The maximum protective effect occurred at about the WHO-recommended level of 150 minutes of moderate-intensity exercise a week.
For Macciochi, the aim should be to move often, in lots of different ways. Prolonged, high intensity exercise can be damaging. “Endurance events, running longer than 90 minutes, can deplete muscle, increase stress hormones and suppress immunity,” she warns. “That’s why marathon runners are more vulnerable to infections during training.”
Manage Stress
The immune system is phenomenally complex but one thing immunologists agree on is the damage caused by chronic stress. When cortisol levels rise – as they do when we are stressed – the immune system is suppressed because the body is saving all its energy for the “fight or flight response”. If this stress is long-term, immunity really suffers.
“Finding ways to manage or reduce stress is key,” says Macciochi, who suggests carving out small pockets of time for things you love. Scientifically proven strategies for managing stress include yoga, meditation, mindfulness and having healthy, positive friendships. Seeking out company can be an immunity boost in itself since loneliness can also make your immune system less robust.
“Looking through an evolutionary lens, it makes sense,” says Macciochi. “[Our] ancestors lived in close proximity where it was easier for germs to spread so the immune system needed to be ready to go. When you live alone, there’s less chance of catching something, so it dampens down the antiviral response.”
She adds: “There are no ‘superfoods’ or ‘magic bullets’ when it comes to building a healthy immunity system, but small tweaks to the way you eat, sleep, exercise and socialise can all help bump it up.”
The Telegraph, London
Make the most of your health, relationships, fitness and nutrition with our Live Well newsletter. Get it in your inbox every Monday.
Most Viewed in Lifestyle
From our partners
Source: Read Full Article