Two pain relief specialists argue that treating chronic pain with opioids can create a cycle of physical and social pain, increasing peoples’ risk of dependence and addiction.

Social rejection hurts, whether it is real or imagined. Nearly everyone will have felt the distress of unanswered messages or phone calls, for example, the perception that someone is avoiding us at a party.
While the physical pain of injury motivates people to avoid further tissue damage and allow time for healing, social pain prompts us to avoid further rejection — and perhaps look elsewhere for companionship.
As a social species, we depend on others for our survival and well-being, so it comes as no surprise that we are wired to find friendship rewarding and rejection hurtful.
In fact, our brains handle physical pain and social pain in a very similar way, with overlapping brain circuits involved in both processes.
This helps explain the two-way relationship between pain and emotional distress, with research showing that each type of suffering can exacerbate the other.
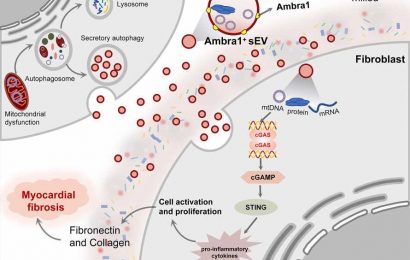
Some evidence suggests that endogenous opioids, which are the body’s pain relievers, play an important role in social bonding.
The downside is that when the chronic use of potent prescription opioids disrupt the endogenous opioid systems, this not only perpetuates pain but may also promote social distress, isolation, and depression.
Writing in the journal Annals of Family Medicine, Mark D. Sullivan and Jane C. Ballantyne from the University of Washington in Seattle, WA, argue that by suppressing the body’s natural system for regulating pain levels and distress, long-term opioid use creates a cycle of physical and social pain.
People can become dependent on the drugs: they take them to avoid the physical, emotional, and social effects of withdrawal. This, in turn, can lead to addiction.
Both Sullivan and Ballantyne prescribe opioids to their patients, but they believe the drugs should be reserved for short-term use that lasts no more than a month or so. They argue that alternative strategies are needed to treat chronic pain; they explain:
“As prescribers of medical opioid treatment, we must recognize that when physical and social pain coexist, long-term opioid therapy is more likely to harm than help … [L]ong-term opioid therapy that lasts months and perhaps years should be a rare occurrence because it does not treat chronic pain well, it impairs human social and emotional function and can lead to opioid dependence or addiction.”
The opioid crisis
According to the Centers for Disease Control and Prevention (CDC), around 1 in 5 adults in the United States experiences chronic pain, which it defines as pain that lasts longer than 3 months or beyond the time when tissue should have healed.
Many of these individuals take opioids prescribed by their doctors to ease the pain, such as codeine, hydrocodone, and fentanyl.
However, more than 11.5 million people in the U.S. aged 12 or older reported misusing prescription opioids in 2016, according to the CDC.
There is a strong association between mental illness and the use — and misuse — of opioids. People with mental health disorders are more likely to receive prescription drugs from their doctors and more likely to misuse opioids.
The drugs not only lead to dependence and addiction; they are also potentially fatal in overdose. The National Institute on Drug Abuse reports that in 2018, 128 people in the U.S. died every day from opioid overdoses.
The physical and emotional effects of opioid dependence are well known, but Sullivan and Ballantyne believe the social effects have been overlooked in America’s opioid crisis.
“Endogenous opioids support the most important and unique human social functions,” they write. “Endogenous opioid systems are crucial for human social bonding, but when damaged, have a role in perpetuating isolation and chronic illness.”
Social isolation
When chronic opioid use compromises the body’s reward and pain relief system, the mutually reinforcing effects of physical and emotional pain create a vicious cycle.
“[R]ather than helping the pain for which the opioid was originally sought, persistent opioid use may be chasing the pain in a circular manner, diminishing natural rewards from normal sources of pleasure, and increasing social isolation.”
To make matters worse, they write, people who choose to use opioids over the long term tend to be those with the most complex forms of chronic pain that contain both physical and social elements.
As a result, these individuals are particularly vulnerable to dependence.
“Survival mechanisms that were already compromised by physical and social injury are compromised further because the [pharmaceutical] opioid can overwhelm the natural endogenous defenses,” they warn.
They believe this may partly explain why people who stop taking opioids after long-term treatment with the drugs are at greater risk of suicide and all-cause mortality.
They conclude:
“This insight into the overlap between physical and social pain should help redirect care for these patients away from opioid treatment that may ultimately worsen their underlying distress and social isolation.”
As an alternative to long-term prescribing of opioids, they advocate multimodal chronic pain care, which combines physical, psychological, and educational interventions.
However, they acknowledge that the implementation and funding of such programs remains a challenge.
Source: Read Full Article