As governments around the world grapple with how to fairly allocate COVID-19 vaccines for maximum protection against the pandemic, an international research team proposes that existing human rights law should act as a guide for politicians and policymakers.
Western’s Maxwell Smith, an expert in public health ethics, co-authored a new study promoting a human rights approach to vaccine distribution that considers social vulnerability along with medical needs in decision-making. The study was led by University of Warwick law professor Sharifah Sekalala.
“National vaccine rollouts should take into account these overlapping vulnerabilities,” said Smith,a professor in Western’s Faculty of Health Sciences and co-director of the university’s Health Ethics, Law, and Policy (HELP) Lab.
As a member of Ontario’s COVID-19 Vaccine Distribution Task Force, Smith helped to develop Ontario’s Ethical Framework for COVID-19 Vaccine Distribution, a blueprint emphasizing that all levels of government have a legal obligation to take preventative steps to stop the spread of COVID-19 and treat people without discrimination.
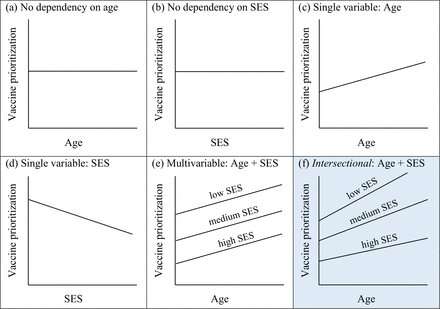
The new study argues similar views with the researchers recommending governments adopt an intersectional approach to understanding how different vulnerabilities and disadvantages affect a person’s health.
Using age and economic status as examples, the study shows how a fair distribution scheme might prioritize populations from a low-income group before populations of similar age from a more well-off background, because economic deprivation, poorer living standards, and worse access to healthcare may place individuals at greater risk from COVID-19.
“In Canada, those who work in informal or insecure jobs, live in overcrowded housing, and have a lower socioeconomic status are overrepresented by racialized populations. This can make it difficult to socially or physically distance, thereby making them more susceptible to infection than people in other circumstances,” said Smith, also a member of the World Health Organization’s Ethics and COVID-19 Working Group. “Data shows the tragic reality is that people from these groups are not only more likely to be infected with COVID-19 but also to die from it.”
Smith and his collaborators argue that a fairer and more effective prioritization system must not only consider vulnerability to infection but also more structural underlying determinants of health that increases their vulnerability to the crisis.
“This is precisely why Ontario has included ‘populations and communities facing barriers related to the determinants of health’ as a vaccine priority group,” said Smith.
The study reviews current approaches to vaccine allocation, from the U.K. age-priority system to Israel’s decision to prioritize healthcare workers and first responders and considers these from a human rights perspective while outlining a model of an ethical, intersectional distribution scheme based on human rights legal principles. “There are three fundamental human rights which need to be reflected in any vaccine distribution program—the right to life, the right to health, and the right to benefit from scientific progress,” said Sekalala.
By recognizing these three fundamental human rights, vaccines should be made available to everyone, says Sekalala.
“If there aren’t enough vaccines available, then they should be given as a priority to people who are more likely to contract COVID-19, to those whose health is at higher risk of being compromised as a result of coming down with COVID-19, and to those who are most likely to transmit the virus,” said Sekalala. “It’s also a key human rights issue that vaccines be distributed without discrimination.”
Source: Read Full Article


