Intensive blood pressure control to a target of less than 120 mm Hg was not associated with a reduction of cerebral perfusion compared with a standard target of less than 140 mm Hg in a substudy of the SPRINT trial.
In fact, contrary to expectations, the intensive group showed an increase in cerebral blood flow, and this was more pronounced in participants with a history of cardiovascular disease.
Results from this secondary analysis of the SPRINT MIND trial were published online in JAMA Neurology on March 7.
“One of the concerns from clinicians about intensive blood pressure lowering has been about effects on the brain and a possible reduction in cerebral perfusion, which could cause all sorts of issues including eventual cognitive impairment and dementia,” lead author of the current analysis, Sudipto Dolui, PhD, University of Pennsylvania, Philadelphia, told theheart.org | Medscape Cardiology.
“These results show that a lower blood pressure, which we know is better for the cardiovascular system, is not bad for the brain in terms of cerebral perfusion — and it may actually be beneficial. This should give clinicians more confidence in lowering blood pressure more intensively,” Dolui said.
“It appears now that intensive blood pressure treatment is beneficial to the brain as well as to the heart,” he added.
The landmark SPRINT trial comparing intensive blood pressure control, targeting a systolic blood pressure less than 120 mm Hg, to a standard treatment target of 140 mm Hg, showed an overall benefit for intensive treatment on cardiovascular morbidity and mortality and cerebrovascular health, including a reduced incidence of adjudicated cognitive impairment, the authors note.
Additionally, among a subset of trial participants who underwent brain MRI, participants randomized to the intensive target had a smaller increase in white matter lesions but greater reduction in total brain volume over a median of 4 years of follow-up, they report.
“The brain has a clever mechanism to keep perfusion levels the same regardless of blood pressure within a certain range of pressures. But there has been concern whether that would still be the case at lower levels of blood pressure, and if aggressive treatment may lower blood pressure below the lower autoregulatory limit and lead to cerebral ischemic injury,” Dolui explained. “This is what we investigated in the current study.”
For the study, 547 patients participating in the SPRINT trial had cerebral blood blow measurements by MRI at baseline and were randomized to either intensive or regular blood pressure lowering. The mean age of patients in this substudy was 67 years, and 40% were women. Follow-up MRIs were performed in 315 patients.
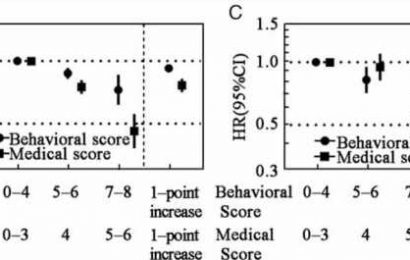
Results showed that mean whole-brain cerebral blood flow increased from 38.90 to 40.36 mL/100 g/min in the intensive treatment group (difference, 1.46), with no mean increase in the standard treatment group (37.96 to 37.12; difference, –0.84 mL/100 g/min), giving a between-group difference of 2.30.
Gray, white, and periventricular white matter cerebral blood flow showed similar changes.
The association of intensive versus standard treatment with cerebral blood flow was generally similar across subgroups defined by age, sex, race, chronic kidney disease, systolic blood pressure, orthostatic hypotension, and frailty.
However, there was one subgroup that showed a difference — those with a history of cardiovascular disease showed larger mean increases in cerebral blood flow associated with intensive treatment (interaction P = .05).
“We found that the group who received intensive blood pressure lowering in SPRINT did not show reduced cerebral perfusion. On the contrary, they actually showed an increase in cerebral perfusion,” Dolui said. “And patients with a history of cardiovascular disease appeared to derive even more benefit in cerebral blood flow from intensive blood pressure lowering.”
Senior author, Ilya Nasrallah, MD, also from the University of Pennsylvania, said, “This is a reassuring study in terms of the decision to treat blood pressure intensively.”
Nasrallah explained that it is critical for the brain to control blood flow to match delivery from the heart to demand.
“There has been a question as to how the brain reacts to a drop in blood pressure. Does the brain of a hypertensive patient get used to the higher blood pressure level and could reducing this pressure cause harm? But our study shows this not to be case,” he told theheart.org | Medscape Cardiology. “We did not see any detrimental effect on brain perfusion of intensive blood pressure treatment and our results suggest that that the brain can adjust to changing blood pressure right down to the lower levels achieved in SPRINT.”
Nasrallah added: “After the compelling cardiovascular outcomes from SPRINT, there was some pushback on concerns about possible adverse effects of intensive blood pressure lowering on other organs such as the brain. And there has been a hypothesis that lowering blood pressure may reduce brain perfusion. But these results should allay those concerns.”
However, he cautioned that clinicians still needed to think about each individual patient and intensive blood pressure reduction may not be appropriated for everyone, such as those who are very frail or who have postural hypotension and are prone to falls.
In their discussion in the paper, the authors say the mechanistic basis for the observed increase in cerebral blood flow associated with intensive treatment remains uncertain but suggests a complex relationship between blood pressure and cerebral blood flow, beyond simply static cerebral perfusion pressure and cerebrovascular autoregulation.
They point out that their results relate to static cerebral autoregulation rather than dynamic autoregulation, which describes cerebral blood flow changes in response to a more rapid change in blood pressure.
“Cerebral blood flow is measured supine, not while standing, and it remains possible that the cerebral blood flow changes when transitioning from sitting to standing pertaining to dynamic autoregulation with intensive therapy can be lower,” they write.
They also note that the association of intensive treatment with brain perfusion stand somewhat in contrast with association with the kidney, where intensive treatment resulted in a greater incidence of acute kidney injury speculated to reflect hemodynamic changes in kidney perfusion.
“This difference may reflect a greater adaptability of cerebrovascular autoregulation to chronic systemic changes or greater tolerance to episodic hypotension relative to the kidney vascular system,” they say.
“New and Encouraging Data”
Commenting on the study for theheart.org | Medscape Cardiology, Michael Weber, MD, professor of medicine at State University of New York, said: “Aggressive treatment of hypertension in middle-aged and older patients can sometimes be associated with dizziness, faintness, and falls. Does this indicate cerebral hypoperfusion? This apparently exciting news suggests that vasodilatory mechanisms beyond traditionally understood brain autoregulation might be activated at low blood pressures.”
Weber pointed out a couple of limitations that suggest caution in interpreting these findings, including several patients not available for follow-up measurements and the issue of measurements being performed with patients in the supine posture, which may not reflect cerebral blood flow when patients are seated or standing.
“Even so, these new and encouraging data are consistent with previous reports from SPRINT that preservation of cognitive function and reduced findings of early dementia were enhanced in patients treated to low systolic blood pressures,” Weber concluded.
Also commenting on the findings, William White, MD, professor emeritus, Calhoun Cardiology Center, University of Connecticut School of Medicine, Farmington, said: “The SPRINT MIND substudy is reassuring that lowering unattended systolic blood pressure to 120 mm Hg was not associated with reductions in cerebral blood flow/perfusion pressures. A substantial concern among clinicians has been that lowering systolic blood pressure too much might lead to increases in orthostatic hypotension (which did occur in SPRINT), syncope, and falls (which did not occur in SPRINT).”
But White noted that the mechanism behind these findings is not known, and since a relatively small proportion of the SPRINT study patients completed the cerebral blood flow studies, the results are not necessarily representative of the entire SPRINT population.
He suggested that another limitation was that patients in the SPRINT MIND substudy had brain imaging for up to another year after the main SPRINT study was stopped prematurely because of cardiovascular benefit, during which time recommendations were made to lower the blood pressure in the standard group to intensive levels for cardiovascular protection. “Hence, it is not clear how the SPRINT-MIND investigators handled this confounding issue,” he added.
Responding to this point, Nasrallah, noted that blood pressure continued to be monitored in the MRI study group after the main SPRINT trial stopped and the difference between the two intervention arms was “pretty much preserved,” so it is not likely that this would be “much of a factor.”
The SPRINT trial was funded by the National Institutes of Health (NIH). Nasrallah reported personal fees from Biogen outside the submitted work. Dolui has disclosed no relevant financial relationships.
JAMA Neurol. Published online March 7. Abstract
For more from theheart.org | Medscape Cardiology, follow us on Twitter and Facebook.
Source: Read Full Article