Superior memory function in a group of older adults dubbed “SuperAgers” may be an indicator that a person is less likely to develop delirium after elective surgery, researchers from Massachusetts General Hospital (MGH) have learned.
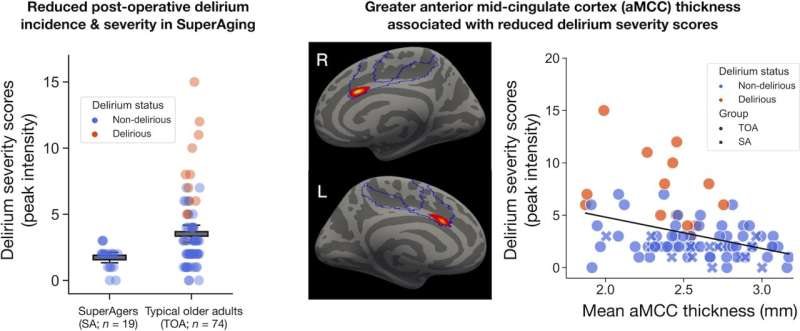
In a study published in Brain Communications, the team reported that SuperAgers, whose memories rival those of young adults, have greater thickness of a frontal portion of the brain known as the anterior mid-cingulate cortex (aMCC), potentially making it a biomarker for predicting the severity of post-operative delirium in older adults undergoing such common elective procedures as total knee and hip replacement, laminectomy (back surgery), and colectomy.
“This remarkable group of SuperAgers has been shown in previous research to be resilient to typical memory decline, but our study found for the first time that ‘SuperAging’ also confers protection against the development and prolongation of delirium after elective surgery,” says co-senior author Alexandra Touroutoglou, Ph.D., director of Imaging Operations at the Frontotemporal Disorders Unit, MGH.
“Because the size of the anterior mid-cingulate cortex is greater in SuperAgers than in typical older adults, it could be a marker for intervention strategies involving therapeutics to mitigate the risk and consequences of post-operative delirium, though more research is needed,” Touroutoglou says.
“The goal of minimizing the risk of delirium becomes particularly important when you consider the growth of the aging population in the coming decades, and the burgeoning number of older people undergoing surgery.”
Delirium is an acute state of confusion and awareness characterized by a disturbance in attention, arousal, and other cognitive functions. Post-operative delirium occurs in as much as 51% of patients 65 years of age or older, substantially increasing their risk of death, institutionalization, and long-term dementia. Indeed, mortality rates among hospitalized patients who develop delirium are as high as those with myocardial infarction or sepsis. Despite the devastating clinical and societal impact, approaches to effective treatment have remained elusive.
In their study, a team of Mass General researchers led by co-author Bradford Dickerson, MD, director of the Frontotemporal Disorders (FTD) Unit at MGH, investigated a cohort of 93 older adults from the landmark Successful Aging after Elective Surgery (SAGES) study, led by collaborator Sharon Inouye, MD.
Through data gathered pre-operatively with a brief memory test, 19 participants were identified as SuperAgers. Structural MRI data were also collected pre-operatively to estimate the cortical thickness of the anterior mid-cingulate cortex, the section of the brain that regulates the amount of effort we expend on various tasks and behaviors.
The results showed that none of the SuperAgers demonstrated full clinical delirium after elective surgery, and that greater pre-surgical thickness of the aMCC was associated with lower severity of post-operative delirium in all participants.
“Given the fact the aMCC exhibits high neural plasticity and that its structure and function can be improved with training, this brain region could be a potential target for intervention strategies designed to prevent delirium,” says Yuta Katsumi, Ph.D., an instructor of Neurology at Mass General Research Institute, and co-first author.
The aMCC, he points out, has shown sensitivity to aerobic exercise in older adults through other studies, with the brain’s gray matter increasing in volume after six months of training.
Source: Read Full Article


