The real-world Zephyr 2 study, which assessed benralizumab for effectiveness in treating severe eosinophilic asthma, was extended with an analysis of a larger population stratified into three cohorts of participants who were aged 12 years or older. Pre- and post-treatment data showed an improvement in asthma control for each group.
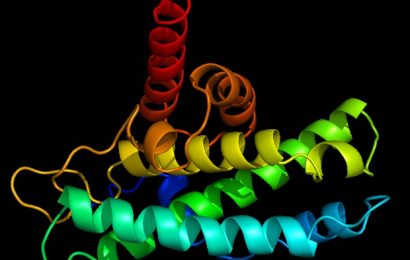
Immunotherapy with monoclonal antibodies designed to block specific inflammatory pathways is a recommended add-on treatment option for adults to manage severe, uncontrolled eosinophilic-dependent (>150 cells/µl) and corticosteroid-dependent asthma. One such biologic, benralizumab, targets the interleukin-5 receptor alpha chain (IL-5Rα).
For asthma patients who had previously been treated with benralizumab, there were significant reductions in exacerbation rates in the ZEPHYR 1 study. However, information regarding benefit associated with specific profiles was limited, warranting a larger study to address effectiveness when considering various blood eosinophil counts, prior treatments with other biologics, or benralizumab use for up to 24 months, Donna Carstens, MD, of AstraZeneca, Wilmington, Delaware, and colleagues write.
Study Details
In the retrospective cohort Zephyr 2 study, which was published in The Journal of Allergy and Clinical Immunology: In Practice, the researchers retrieved deidentified patient information from medical, laboratory, and pharmacy US insurance claims records from the PatientSource and DiagnosticSource databases and compared asthma exacerbation rates before and after treatment with benralizumab.
Age, asthma diagnosis, number of exacerbations, and number of benralizumab treatment records within specified periods were used to identify a total of 1795 participants for inclusion in the study. The index date for establishing before-treatment and after-treatment index time intervals of 12 months each was defined as the day after the initial benralizumab treatment occurring between November 2017 and June 2019.
The cohort was stratified into three nonmutually exclusive groups consisting of 349 patients who had switched primarily from either omalizumab or mepolizumab biologics to benralizumab; 429 patients subdivided by closest to the index date blood eosinophil counts of <150, ≥150, 150-299,<300, and ≥300, and 419 patients with post data collection extended beyond 12 months to 18 or 24 months.
Similarities in baseline patient characteristics that were were observed across the three cohorts included a mean age range of 51–53 years, preponderance of women (67% to 69%), obesity diagnosis (31.5% to 32.9%), and a mean Charlson Comorbidity Index of 1.47 – 1.52. Allergic rhinitis was the most frequently reported (60% to 67%) comorbidity, followed by hypertension and gastroesophageal reflex.
Effectiveness
Benralizumab was found to be a significantly effective treatment for managing severe eosinophilic asthma for all three evaluated cohorts, as evidenced by reductions in asthma exacerbations post-index compared to pre-index. Specifically, the exacerbation rate for all five subgroups of the blood eosinophil cohort significantly decreased from the pre-index 3.10 – 3.55 person per year (PPY) rate to a 1.11 – 1.72 PPY post-index rate, equivalent to a 52% to 64% decrease in exacerbations (P < .001 for all pre-index vs post-index comparisons).
Comparable reductions also occurred with the cohort in which the biologic treatment was changed to benralizumab. A greater effect was observed when the switch was made from omalizumab to benralizumab with a pre-post PPY rate reduction of 3.25 to 1.25 (62%) than when the switch was made from mepolizumab (pre-post PPY rate reduction was 3.81 – 1.78 [53%], but both resulted in significant post-treatment improvements (P < .001).
Results from the extended follow-up analysis cohort showed consistency for significant exacerbation rate decline going from a pre-index rate of 3.38 PPY down to 1.34 PPY (60% rate reduction vs pre-index) in the first 12 post-index months, continuing to decline to 1.18 PPY (65% reduction) over the following six months (both significant at P < .001).
Likewise, the results from the extended follow-up 24-month subgroup presented significant down trending exacerbation rates from pre-index 3.38 PPY to 1.38 (comparative 59% reduction) for the first 12 months continuing down to 1.08 PPY (68% reduction) over the 12–24 month post-index period (both P < .001). In the first and second 12 post-index months for the 24-month subgroup, 39% and 49% of the patients, respectively, experienced no exacerbations
Following treatment with benralizumab, in addition to the observed decline in asthma exacerbation rates, the need for concomitant asthma medications was also significantly reduced for all three cohorts.
This retrospective ZEPHYR 2 study contributes evidence supporting the significant effectiveness of benralizumab in improving disease management for “specific subsets of severe asthma patients that are frequently seen in real-world practice and may be excluded from clinical trials,” according to the authors. The treatment resulted in reduced rates of asthma exacerbations with defined standards for hospitalizations, visits to emergency department or urgent care, or outpatient visits with separate exacerbations occurring at ≥14 days, as reported in database records. Reduction in the rate of asthma exacerbations when benralizumab is switched for another biologic increases the disease management options for achieving optimal patient care, the authors add.
The authors have financial relationships with AstraZeneca, the source of funding for the study.
J Allergy Clin Immunol Pract. Published online May 3, 2023. Abstract
Follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article