Researchers at Fudan University in Shanghai, China have developed three different techniques that successfully replace almost all malfunctioning microglia—each technique with its own advantage in application.
The researchers published their findings on Aug 11, 2020 in Cell Reports.
Microglia are a specialized type of immune system cell that are found throughout the central nervous system (CNS), including brain, retina and spinal cord. Their main job is to protect the neurons of the central nervous system by gobbling up pathogens, cancer cells, foreign substances and cellular debris. They are sort of like a vacuum cleaner that the immune system uses to keep the central nervous system clean. Malfunctioning microglia are associated with many neurological diseases such as Alzheimer’s, ALS and Parkinson’s. Gene therapy to replace defective microglia-related genes with properly functioning ones offers tremendous potential to alleviate or perhaps one day even eliminate such diseases.
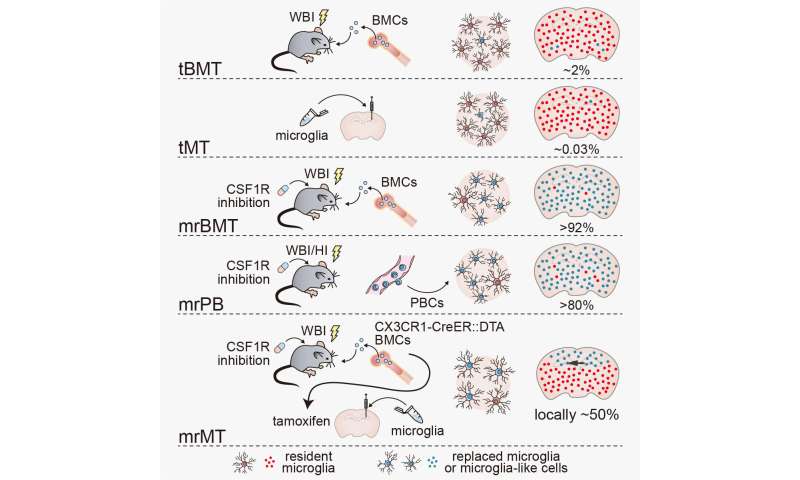
However, up till now, such efforts in the lab or testing on animals have largely failed long before any clinical trials on humans. Attempts at transplants of microglia or of bone marrow (because bone marrow is the main location in the body of production of new stem cells that can differentiate themselves into microglia) only end up replacing up to 5 percent of the faulty microglia. Other strategies that have been more successful when tested on mice require the animal to have a suppressed immune system and still be at the neonatal stage of life. This means that it is impossible for such a strategy to be used in any real-world clinical application for humans.
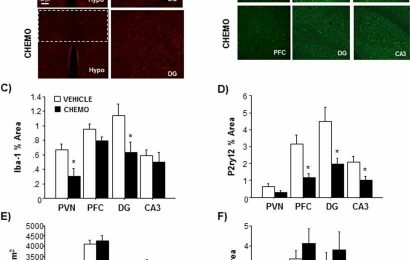
In an earlier study, the same team had noticed that when drugs had been used to almost completely eliminate all existing microglia, the few that remained had an astonishing ability to proliferate. This suggested to them that to get any microglia, native or transplanted, to substantially proliferate, you need the trigger of a completely empty microglial ‘niche’ into which new microglia grow.
So the researchers replicated this effect by feeding normal adult mice for two weeks a diet that included a drug that inhibits the production of a molecule necessary for microglial survival. Only after all the microglia were wiped out, did the researchers attempt a bone marrow transplant. This time, some 93 percent of microglia were replaced in the brain, 99.5 percent in the retina, and 93 percent in the spinal cord.
They call this technique microglia replacement—because pretty much all the old microglia get replaced by new ones—by bone marrow transplant, or mrBMT.
“We pronounce the acronym for the technique ‘Mister BMT’,” said Bo Peng, the corresponding author and professor from the Institute for Translational Brain Research at Fudan University. “It’s a cute name, but it makes it easy to say and to remember.”
Despite the impressive replacement efficiency of mrBMT, bone marrow cells are rather scarce in clinical practice. So the researchers tried the same technique of eliminating existing microglia before transplant, but now with peripheral blood cells (PBC) instead of bone marrow cells. (Peripheral blood is the blood that circulates in much of the body, distinct from the blood cells that stay enclosed in the liver, spleen and other areas that have their own specialized type of blood). Such blood is abundant and easily acquired.
This second technique, called mrPB, (similarly pronounced “Mister PB”), replaced 80 percent of the microglia. So between the two techniques, there is trade-off: mrBMT offers close to full microglia replacement, but donor sources are hard to come by, while mrPB offers donor sources that are easy to come by, but the microglia replacement is slightly less efficient.
Sometimes though, a patient might need only the microglia in a specific part of the brain to be replaced without affecting the rest of the brain. So the researchers tweaked their concept still further. Using mrBMT first to replace resident cells with chemically sensitive microglia. After that, tamoxifen was applied to induce a fragment of a diphtheria toxin to kill off the replaced mrBMT cells. Meanwhile, they directly injected normally functioning microglia, which do not respond to tamoxifen, into a specific brain region with a syringe. While mrBMT and mrPB microglia still have some slight differences with regular microglia, the third technique, mrMT produces microglia almost indistinguishable from the normal kind.
Source: Read Full Article