In a recent study posted to the bioRxiv* preprint server, researchers revealed that the nucleotide-binding oligomerization domain-like receptors or NOD-like receptors (NLR) family pyrin domain containing 3 (NLRP3) inflammasome is activated by the exosomes from plasma in coronavirus disease 2019 (COVID-19).
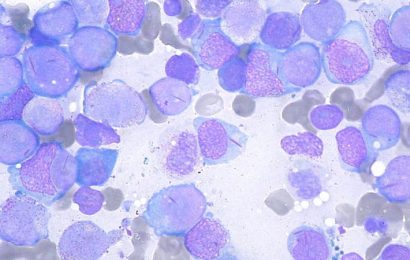
 Study: Circulatory exosomes from COVID-19 patients trigger NLRP3 inflammasome in endothelial cells. Image Caption: Jason Drees/Shutterstock
Study: Circulatory exosomes from COVID-19 patients trigger NLRP3 inflammasome in endothelial cells. Image Caption: Jason Drees/Shutterstock
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), the etiologic agent of the COVID-19 pandemic, has caused more than 396 million global infections so far. With over 10.3 billion doses of SARS-CoV-2 vaccines administered worldwide, COVID-19 infections continue to rise as the mutant variants of the virus emerge with enhanced pathogenicity. Albeit vaccinated individuals can contract SARS-CoV-2, it has been observed that the vaccine-elicited immunity can protect from severe disease outcomes.
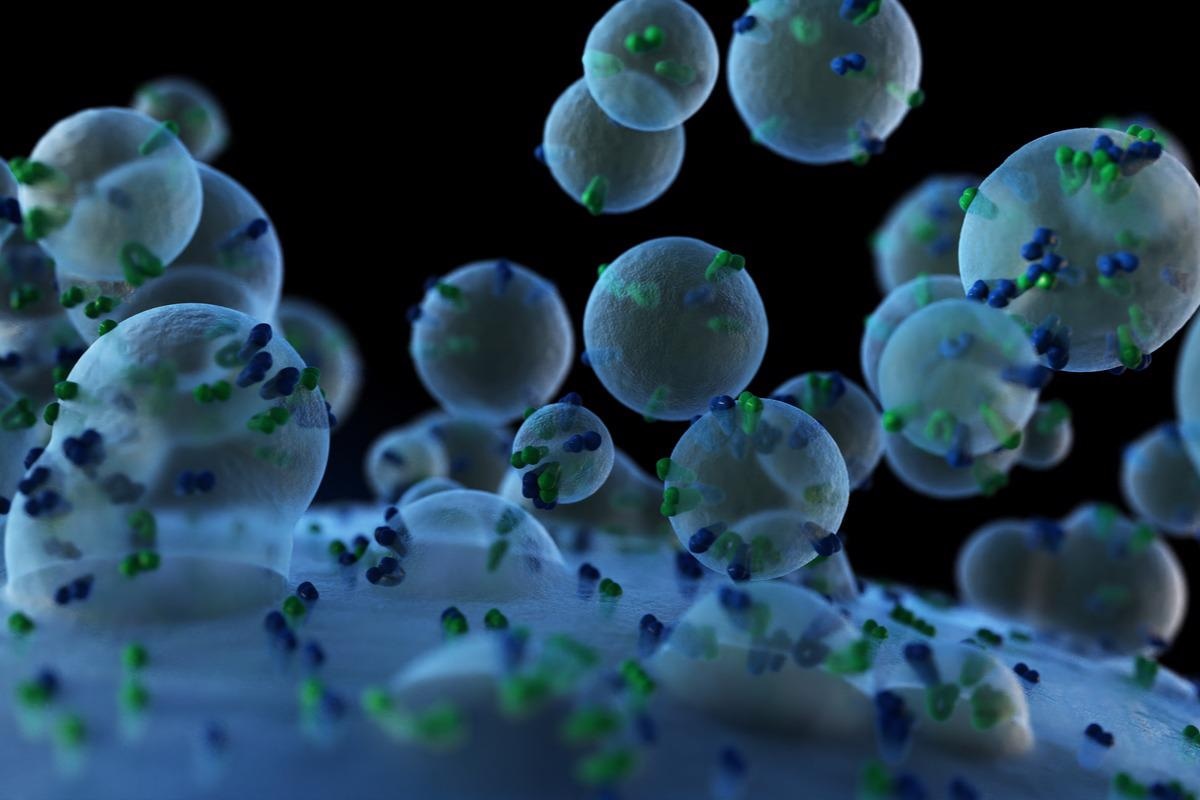
Inflammasomes are multiprotein complexes in the cytoplasm implicated in eliciting cellular responses against external stimuli, and NLRP3 is one such inflammasome involved in inflammatory and antiviral responses. The oligomerization of NLRP3 proteins in the cytoplasm creates NLRP3 inflammasome. Exosomes are extracellular membrane-bound vesicles secreted from cells as a consequence of the internal budding of endosomes. These exosomes are involved in cell communication and transport of biomolecules and also play an important role in disease pathogenesis and antiviral responses.
Studies have reported that a severe COVID-19 infection causes inflammatory reactions, venous thromboembolism (VTE), cytokine storm, multiple organ failure, and coagulopathy among others. Endothelial cells act as a selectively permeable barrier to blood, controlling inflammation, thrombosis, and proliferation of vascular smooth muscle. Reports suggest that endothelial cell-related inflammation occurs during SARS-CoV-2 infection, but its molecular mechanisms are poorly understood.
The study
In the present study, researchers examined the responses of endothelial cells to plasma exosomes from severe COVID-19 patients. Exosomes were isolated from the plasma collected from COVID-19 patients admitted to the intensive care unit (ICU) and from healthy subjects.
Human microvascular endothelial cells (HMEC-1) and liver endothelial cells (TMNK-1) were incubated with exosomes from healthy persons and infected patients to understand the formation of inflammasomes.
Findings
HMEC-1 exposed to exosomes from severe COVID-19 patients demonstrated significantly higher messenger ribonucleic acid (mRNA) levels of NLRP3, pro-caspase-1 (CASP1), and pro-interleukin-1β (pro-IL-1β) than the cells treated with exosomes from healthy individuals. Similarly, TMNK-1 cells showed higher transcription of these genes. Incubating THP-1 cells (a cell line from acute monocytic leukemia patients) with exosomes from healthy or infected individuals had no such reproducible effect on NLRP3 gene expression. This suggests that NLRP3 inflammasome genes from endothelial cells of two different organs could be stimulated by exosomes from COVID-19 patients.
Activated inflammasome converts pro-caspase-1 into its active form by proteolysis. The Western blot analysis confirmed increased levels of cleaved caspase-1 in the endothelial cells exposed to COVID-19 exosomes when compared to the cells exposed to exosomes from healthy subjects. It is known that inflammasome-activated cells secrete caspase-1, and the authors further investigated and observed high caspase-1 levels in the culture media of COVID-19-exosome-treated endothelial cells.
Pro-IL-1β is proteolytically cleaved by an activated caspase-1 which activates it into a functionally active and mature cytokine (IL-1β). The researchers assessed the levels of active IL-1β by an enzyme-linked immunosorbent assay (ELISA) and observed that the exposure of exosomes from COVID-19 patients had greatly enriched IL-1β levels in the media of both HMEC-1 and TMNK-1 cells, suggesting that COVID-19 exosomes had triggered the synthesis of IL-1β in endothelial cells through NLRP3 inflammasome activation.
Conclusions
The findings of the present study showed that exosomes from severe COVID-19 patients triggered the transcription of NLRP3, caspase-1, and IL-1β genes. Elevated levels of active caspase-1 secreted into the medium, suggest that COVID-19 patient exosomes induced the NLRP3 inflammasome formation in endothelial cells. Since caspase-1 activates pro-IL-1β into an active form by proteolytic cleavage, the authors suggest that NLRP3 inflammasome formation stimulated the synthesis of inflammatory cytokine (IL-1β) causing endothelial cell dysfunction.
Endothelial cell dysfunction has been suggested to cause multi-organ failure in various viral infections. Although prior studies found pulmonary endothelial cell dysfunction in severe COVID-19 cases, the present study showed that endothelial cells from distant organs can become inflamed due to exosomes from COVID-19 patients with severe disease.
Thus, based on the observations, the authors propose that exosomes may serve as mediators of endothelial cell dysfunction via NLRP3 inflammasome activation and could stimulate inflammation in several organs during severe COVID-19 disease.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Subhayan Sur, Robert Steele, T. Scott Isbell, Ranjit Ray, Ratna B. Ray. Circulatory exosomes from COVID-19 patients trigger NLRP3 inflammasome in endothelial cells. bioRxiv. doi: https://doi.org/10.1101/2022.02.03.479081 https://www.biorxiv.org/content/10.1101/2022.02.03.479081v1
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Acute monocytic leukemia, Assay, Blood, Cell, Cell Line, Coronavirus, Coronavirus Disease COVID-19, covid-19, Cytokine, Cytoplasm, Endothelial cell, Enzyme, Exosome, Exosomes, Gene, Gene Expression, Genes, immunity, Inflammasome, Inflammation, Intensive Care, Interleukin, Leukemia, Liver, Membrane, Muscle, Nucleotide, Pandemic, Proliferation, Respiratory, Ribonucleic Acid, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Thromboembolism, Thrombosis, Transcription, Vaccine, Vascular, Venous Thromboembolism, Virus, Western Blot

Written by
Tarun Sai Lomte
Tarun is a writer based in Hyderabad, India. He has a Master’s degree in Biotechnology from the University of Hyderabad and is enthusiastic about scientific research. He enjoys reading research papers and literature reviews and is passionate about writing.
Source: Read Full Article