An advanced imaging approach developed at the University of Virginia School of Medicine could let surgeons determine the best target in the brain to stop epilepsy seizures, new research suggests.
UVA’s approach could improve patient outcomes and open the underused surgery to patients who are now ineligible, the research team reports.
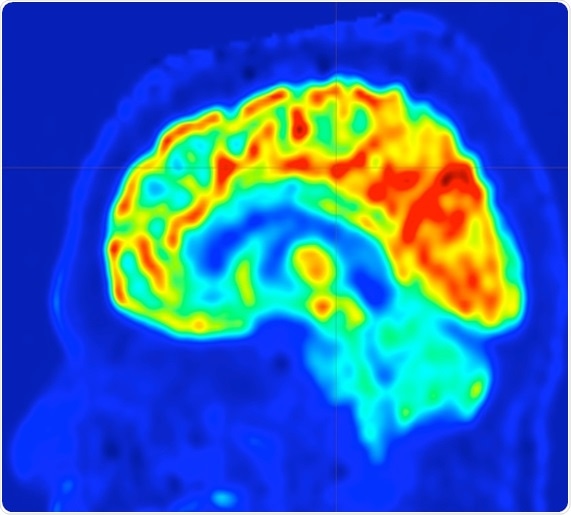
This imaging approach is significant as it creates 4D brain maps which offer additional sensitivity over standard-of-care imaging by revealing rates of glucose uptake rather than final absolute glucose uptake. This imaging approach might be beneficial as it may offer non-invasive localization of potential epileptic foci.”
Bijoy Kundu, PhD, Imaging expert, UVA’s Department of Radiology and Medical Imaging and UVA’s Department of Biomedical Engineering
Preventing epilepsy seizures
UVA’s new approach uses an enhanced form of positron-emission tomography (PET) to measure glucose use in the brain. This allows doctors to pinpoint the trouble spot in the brain that is triggering seizures. Once that spot is identified, it can be removed surgically, stopping the seizures.
PET scans have been used in the past to identify epilepsy trouble spots, but such scans have limited accuracy and often fail to identify an appropriate target. So a team of UVA researchers, backed by the UVA Brain Institute, developed the new approach, called “parametric dynamic FDG-PET imaging” (p-dFDG-PET).
To assess if the new approach offers improved sensitivity and accuracy, Kundu and UVA neurologist Mark Quigg, MD, launched a small pilot study. They performed scans on seven participants for whom traditional PET imaging had failed to identify a target. The results were encouraging: The technique located appropriate trouble spots in all seven.
“In the one patient who underwent successful surgery, p-dFDG-PET predicted the surgical target,” the researchers write in a new scientific paper outlining their findings. “In contrast, in the one patient who underwent unsuccessful surgery, p-dFDG-PET indicated a different surgical target than the one undertaken.”
The researchers say a larger study is needed to more fully assess the potential of UVA’s new approach. But if the technique works as well as the early results suggest, it could transform epilepsy care for many patients. Any hospital with a PET scanner could easily adopt UVA’s approach, the researchers say.
Too often patients with intractable epilepsy turn away from transformative epilepsy surgery when invasive procedures are required to locate the ‘bad spot’ or the epileptic focus. Dynamic PET, as an addition to the noninvasive toolkit, can expand the number of epilepsy surgery candidates.”
Mark Quigg, MD, UVA neurologist
About the epilepsy research
The researchers shared their findings at October’s World Molecular Imaging Congress and are preparing a manuscript for peer-reviewed publication. The research team consisted of Vikram Seshadri, Katherine A. Zarroli, Robert S. Schetlick, James C. Massey, Jose M. Reyes, Thomas J. Eluvathingal Muttikal, James T. Patrie, Stuart S. Berr, Nathan B. Fountain, Kundu and Quigg.
The work received financial support from the UVA Brain Institute. UVA’s Department of Biomedical Engineering is a collaboration of the School of Medicine and the School of Engineering and Applied Sciences.
University of Virginia Health System
Posted in: Device / Technology News | Medical Condition News
Tags: Brain, Brain Surgery, Epilepsy, Glucose, Hospital, Imaging, Medical Imaging, Medicine, Molecular Imaging, Radiology, Research, Surgery, Tomography
Source: Read Full Article


