Researchers from the Multidisciplinary Institute of Medium Study Institute Ramón Margalef (IMEM) from Alicante University (UA), in collaboration with epidemiologists from the National Centre for Tropical Medicine of the Carlos III Health Institute of Madrid, have developed the first open modeling tool with which to compare different COVID-19 spreading scenarios. Another step forward in this scientific race to understand the fast spreading of this infectious disease and to generate scenarios to test the effect of different control measures against the coronavirus.
Thanks to this collaboration, it is possible to calculate the increase or decrease of infected people per day by presenting different scenarios: “What would happen if we restricted the social life of the population more or less, if we extended the isolation measures in time, or if mass vaccinations were conducted, among other propositions of interest,” explains IMEM researcher and professor at the Department of Ecology of the UA, César Bordehore.
The objective of this tool is to provide an open model—using the STELLA program of Iseesystems—which makes it possible to evaluate the behavior of COVID-19 in different scenarios by choosing the area and region. “Our intention is not to generate a model to accurately predict the evolution of the disease, but to compare possible scenarios, evaluate their effects and decrease new infections and, ultimately, the number of deaths. All by open sharing a tool that is easily adaptable to each area,” he adds.
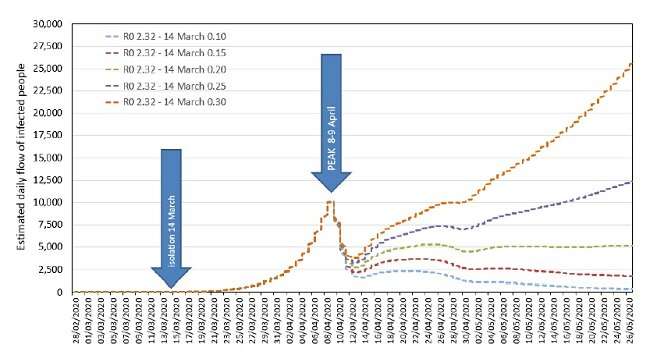
Specifically, experts in Population Dynamics, Medicine and Epidemiology who have taken part in designing this COVID-19 spreading model, have worked, based on official data from the Ministry of Health, Consumption and Social Well-being, on different models and scenarios according to different degrees of isolation, noted as R0, which indicates the speed of spreading (0 is total confinement and 2.32 is the initial R0 before the measures implemented on 14 March 2020).
Scenarios
As UA researcher César Bordehore explains, “our model notes that the peak of infected people will take place around 8 or 9 April, which is why it is essential, as of this date, to maintain very restrictive isolation measures to minimize the daily flow of new COVID-19 cases.” In this sense, regarding the social distancing measures, the model detects and quantifies the positive effect of decreasing R0, in other words, of strengthening the measures and paralyzing all activity to contribute towards increasing the number of infections, especially those caused by people without symptoms.
“The model has verified that although the state of alarm was decreed on 14 March, establishing a series of isolation measures, these have not been severe enough to decrease the number of infections as much as could have been possible. The strengthening of isolation measures implemented as of March 30 precisely sought to further decrease the spreading rates. However, the importance of strengthening the control measures of new infections in home surroundings must be stressed and, given the high percentage of infected healthcare staff, to protect said staff more than ever, minimizing new cases and addressing the saturation of the healthcare system,” highlights the expert.
Furthermore, the researchers have verified what would happen if a policy of diagnostic tests for the whole population had been adopted. Bordehore explains that “the best results are obtained by testing people with a high risk of infection, such as healthcare workers, those who are in contact with sick people or in old people’s homes. In fact, the WHO is insisting on the need to increase the number of tests, especially so that people without symptoms do not infect those around them.”
Another scenario exhibited in this model is what would happen if the isolation measures ended ten days after being implemented. As detailed in the study, these measures should not stop as there would still be infected individuals among the population who could infect others who are not immune to the virus.
Open access
One of the strengths of this model is that it has been created in open access so that it can be adapted to specific situations by any researcher with a computer and internet access. The COVID-19 spreading model, says the UA expert, “can be a powerful tool to educate and convince people about the importance of adopting early and prolonged social distancing approaches.”
In this sense, he adds that “we believe that this tool could be specifically convenient for researchers and healthcare staff in countries with low and medium income, where population models are not as developed and implemented. Thousands of cases of COVID-19 have already been detected in countries of sub-Saharan Africa according to data from the WHO, which is why being able to work with this modeling tool makes it possible to adopt the best decisions when addressing the coronavirus epidemic and help visualize the need to enforce these measures.”
Collaboration
The COVID-19 spreading study model designed by the team of researchers of the UA and the Carlos III Health Institute is constantly being verified and updated. “Our intent, says Bordehore, is to enhance this data with other institutions and scientists that have more accurate parameters to be able to generate other simulation models and compare new scenarios to delve into the development of infections caused by COVID-19.”
Source: Read Full Article


