An over-the-counter cough suppressant can knock some heart cells back into rhythm, a finding that may lead to a new way to treat a rare heart condition called long QT syndrome.
The discovery was made with the help of stem cells from patients with the disorder.
In people with long QT syndrome, heart cells are not always ready to produce the next beat, a situation that can knock the heart out of its normal rhythm, which may be life-threatening. For many people with long QT, no treatment can correct the heart cells or prevent arrythmia.
Understanding how human heart arrythmias can be stopped is difficult to study with mice, so Columbia’s Masayuki Yazawa, Ph.D., turned to patient-derived reprogrammed stem cells, which can be made into heart cells in the lab.
Heart cells in a dish
The cough suppressant discovery began several years ago when Yazawa found that heart cells in the lab would resume a normal rhythm when a certain enzyme was inhibited. But the drugs used to inhibit the enzyme also had other unintended effects, such as liver toxicity.
“We had to find alternatives,” says Yazawa, assistant professor of rehabilitation & regenerative medicine at the Columbia University Vagelos College of Physicians and Surgeons and also a core faculty member of Columbia Stem Cell Initiative.
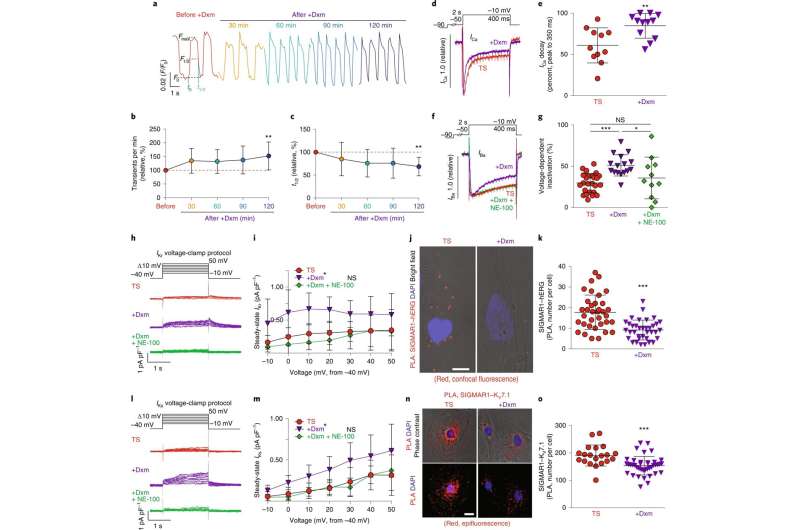
Yazawa’s team reviewed published studies for ideas and learned that the enzyme could be inhibited through an intermediary molecule inside heart cells called SIGMAR1. Further reading suggested that SIGMAR1 could be targeted by a cough suppressant, dextromethorphan.
Heart cells on cough medicine
In the new study, Yazawa’s team found that the cough suppressant, when added to heart cells, successfully prepared the heart cells for the next beat and soothed the cells’ irregular rhythm.
The cough suppressant reset heart cells from people with Timothy syndrome, a genetic disorder that also causes other heart abnormalities, and from people with more common forms of long QT syndrome.
Yazawa cautions that it’s premature to use dextromethorphan to treat long QT patients; the drug has a short half-life and would have to be used long term, which might still have unknown adverse side effects.
“But our study shows that drugs targeting SIGMAR1 have potential to treat a wide array of patients with long QT syndrome,” says Yazawa, “and we will continue to look for better options.”
Says Emmanuelle Passegué, Ph.D., Alumni Professor of Genetics and Development and director of the Columbia Stem Cell Initiative: “This is a beautiful example of how patient-derived reprogrammed stem cells (or induced pluripotent stem cells) can be used to discover new treatments for uncurable conditions and improve patient health.”
Source: Read Full Article


