Treatment for HIV has improved tremendously over the past 30 years; once a death sentence, the disease is now a manageable lifelong condition in many parts of the world. Life expectancy is about the same as that of individuals without HIV, though patients must adhere to a strict regimen of daily antiretroviral therapy, or the virus will come out of hiding and reactivate. Antiretroviral therapy prevents existing virus from replicating, but it can’t eliminate the infection. Many ongoing clinical trials are investigating possible ways to clear HIV infection.
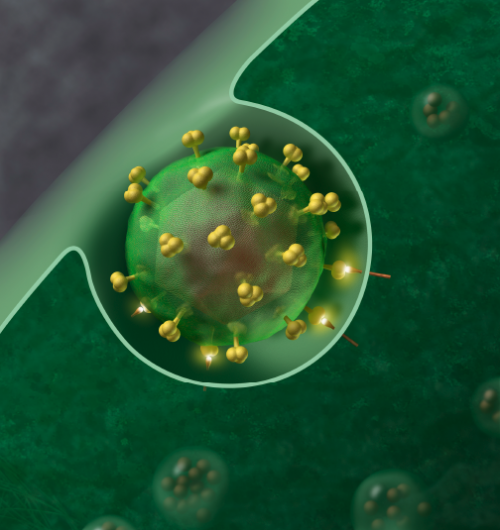
In a study published Feb. 4 in the journal Science, researchers at Washington University School of Medicine in St. Louis have identified a potential way to eradicate the latent HIV infection that lies dormant inside infected immune cells. Studying human immune cells, the researchers showed that such cells have a natural alarm system that detects the activity of a specific HIV protein. Rather than attack the virus based on its appearance, which is the basis of most immunotherapies, this strategy is to attack the virus based on what it is doing—vital activities that are required for the virus to exist.
HIV is nearly impossible to eradicate because the immune system can’t keep up with its unusually rapid mutation rate, constantly changing the way it looks to evade immune attack—akin to a spy quickly changing appearance to evade authorities. Just as the body’s immune cells learn to recognize one manifestation of the virus, it already has changed into multiple new disguises.
“When we identified a part of the immune system that could recognize and attack a core function of the HIV virus—rather than what it looks like—it was really exciting,” said senior author Liang Shan, Ph.D., an assistant professor of medicine. “An analogy might be that it’s relatively easy to change clothes or hairstyle to go undetected, but it’s impossible to conceal running. This is exciting because it raises the possibility of clearing all the dormant virus in a single patient—no matter how widely mutated—based on something all the viral variants have in common. For patients, even if they are consistent with therapy and experience no symptoms, having a treatment that could change their HIV status from positive to negative would have a massive impact on their lives.”
This strategy relies on detecting the activity of a specific protein—called HIV protease—that the virus requires to replicate and spread.
The researchers identified a natural alarm system—found inside human immune cells and called the CARD8 inflammasome—that recognizes active HIV protease and triggers a self-destruct program to eliminate the infected cell. Unfortunately, HIV can exist a long time in the cell without ever tripping the alarm. When inside cells, HIV protease is inactive, lying low, and the CARD8 inflammasome can’t detect it.
“The virus is smart,” Shan said. “Normally, HIV protease doesn’t have any function inside infected cells. Viral protease is only activated once the virus leaves the infected cells. Outside the cells, there is no CARD8 to sense the active protease.”
Shan and his colleagues showed that certain drugs force HIV protease to show itself prematurely, when the virus is still inside the immune cell. There, active HIV protease triggers the CARD8 inflammasome, setting off a chain of events that destroys the infected cell and the virus along with it.
“We found that our immune system can recognize this key protein function—not the protein sequence, which the virus changes constantly through mutation,” Shan said. “HIV protease can’t mutate because its function is required to complete the virus’s life cycle. Otherwise, it’s a dead virus. HIV protease’s specific action for the virus is also the specific action that sets off CARD8. Our findings show that our immune system can recognize a virus’s protein function and, under the right circumstances, use that information to kill HIV-infected cells.”
One of the drugs that forces HIV protease to become active is called efavirenz (brand name Sustiva). It is part of a class of drugs called non-nucleoside reverse transcriptase inhibitors (NNRTIs), which have been used to treat HIV since the 1990s.
“We’ve long used this class of drugs to block HIV from inserting its genetic material into new cells,” Shan said. “That’s their day job. But now, we have learned they have a second job—activating HIV protease inside the infected cell. When we treat HIV-infected human T cells with this drug, the protease becomes activated before the virus successfully leaves the infected cells. This triggers the CARD8 inflammasome, and the infected cells die within hours. This is a potential route to clearing the virus that we have never been able to completely eliminate.”
But the researchers also found that efavirenz and other NNRTIs won’t activate HIV protease unless the virus is awake, as Shan puts it. And in patients on HIV therapy, the virus is dormant. Many clinical trials seeking cures for HIV use a shock-and-kill method, waking up the virus with one drug and then attacking it with one of a variety of investigational strategies. Any clinical trial evaluating NNRTIs, or similar drugs that work the same way, as a potential approach for clearing HIV infection would require this shock-and-kill strategy.
The researchers also showed that the CARD8 inflammasome can trigger the death of human immune cells infected with HIV subtypes from around the world, including strains common in North America, Europe, Africa and Asia.
Source: Read Full Article


